Abstract
Clinical use of a food inventory to identify maternal underreport on children‚??s food intake: experience of a reference center in Brazil
Author(s): Ribeiro, Letícia W; Ricci, Raquel; Maximino, Priscila; Machado, Rachel HV; Bozzini, Ana Beatriz; Ramos, Cláudia C; Malzyner, Gabriela; Fisberg, Mauro
Background: Feeding Difficulties (FD) are a common problem in childhood, and dietary assessments are extremely important to evaluate food consumption and selectivity patterns. In clinical practice, it is often observed that caregivers have an exacerbated perception of the severity of their children’s FD and this may impact on dietary reports.
Objectives: To compare the variety of foods consumed by children with FD under maternal perception to the evaluation performed by nutritionist using a food inventory in association with traditional methods.
Methods: It is a cross sectional study with 119 motherchildren pairs, with complaints of FD followed at an outpatient service in São Paulo, Brazil. Data collected consisted of demographics, maternal caregiving style, responsibility over feeding the child, perception of children’s feeding diversity (expressed in numbers, taken from a self-explanatory food inventory), presence of organic disease, type of FD, BMI Zscore, and actual repertoire of foods consumed (expressed in numbers, assessed by the nutritionist after evaluating the food inventory). The inventory provided information aboutthe food items the child accepts without rejection, used to accept but now rejects, and completely rejects. Spearman correlation and Lynn’s coefficient of variation, ANOVA and T-student tests were used, with a 5% significance level.
Results and discussion: Overall food diversity ranged from 16 (p25%) to 30 (p75%) different types of foods. Maternal perceived food diversity ranged from 4,3 to 14,5 (p25-75). Around 23,7% of children were considered highly selective (less than 15 types of foods) (p=0,000). Maternal perception underestimated that assessed by the nutritionist in 2,2 times, with low reproducibility between these two variables (r=0,14). Both maternal perception and professional assessment did not vary according to age, organic comorbidities, gender, maternal parity, feeding style or responsibility over feeding routines (p>0,49). Findings enhance the importance of parental behavioral interventions and of the use of dietary research methodologies which are complementary to already validated strategies.
Conclusions: There was maternal underestimation on the quantity of foods accepted by children with FD. The data reinforce the need for family orientation about the expectations regarding the feeding practices and preferences of their children.
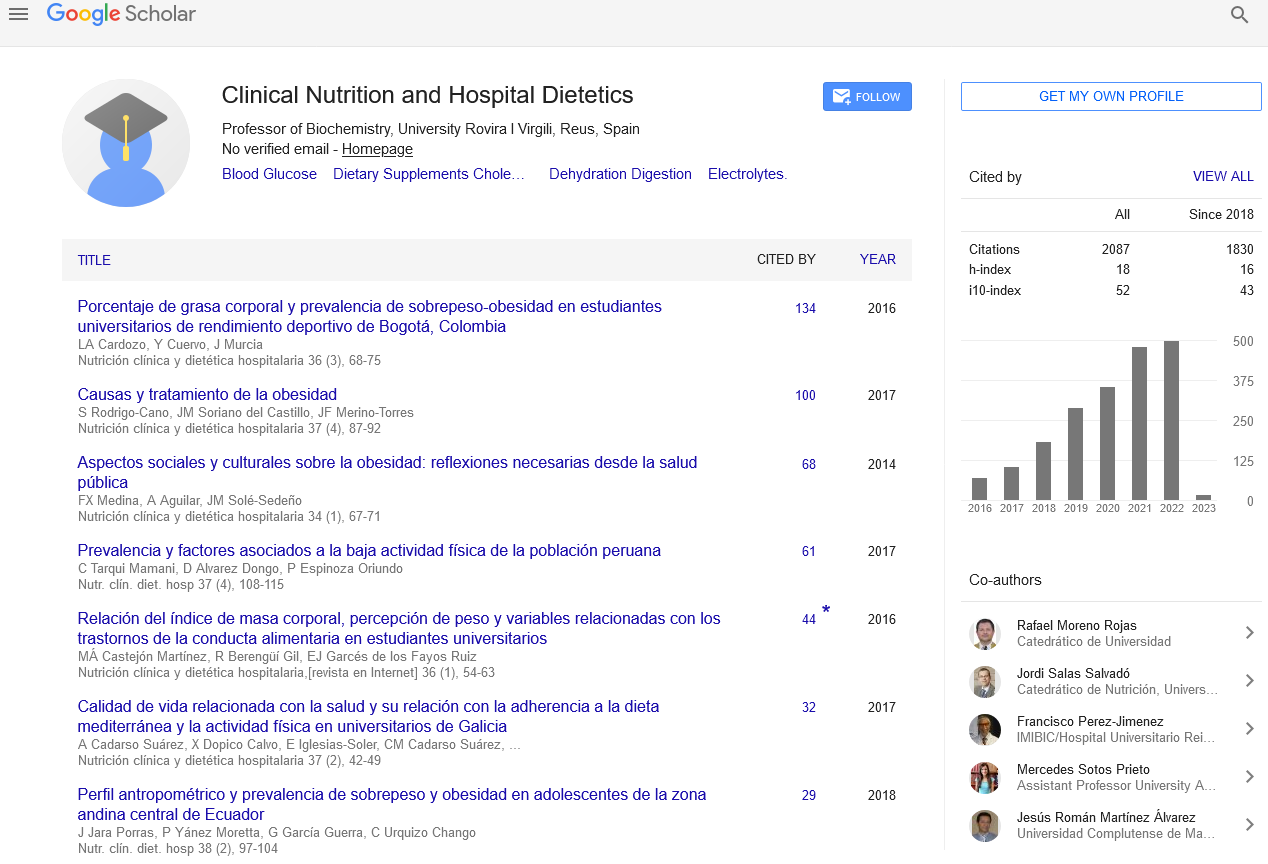
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics