Abstract
Effect of measures to protect breastfeeding described by high rates in a third-level neonatology unit
Author(s): Sánchez Ansede, Alba; Moreno Moreno, Lidia; Linares Ocampo, Paula; Fernández Pombo, Carmen Neri; Sancho GarcÃÂa, Leonor; ÃÂvila ÃÂlvarez, Alejandro; Eiriz Barbeito, Dolores
Introduction: Protecting the breastfeeding of those mothers with a desire to breastfeed guarantees better health outcomes in the neonate both in the short and long term.
Objectives: To know the effect of breastfeeding protection measures on the rate of exclusive breastfeeding at discharge and the related profile.
Methods: Observational and retrospective study conducted in a Third Level Neonatal Unit. A sample of 171 infants recruited from January 26, 2017 and July 20, 2018 was available. Criteria for inclusion: express wish of the mother to breastfeed as reflected in the birthsheet and the existence of the Breastfeeding Card of the newborn of the Unit. Pearson Chi-square test and Student's t test were applied as appropriate, considering a significant value of p <0.05.
Results: The rate of exclusive breastfeeding was 63.8% (54.4% direct or chest administration and 9.4% deferred administration by syringe, as a non-interference method, or bottle. The 10% offered formula and 25.7% mixed breastfeeding. As factors related to the establishment of breastfeeding, there was a higher incidence of this in the neonates from the home compared to those admitted from birth (25.8% vs 9.7%, p = 0.012), in preterm infants older than 32 weeks compared to the younger ones (71% vs. 29%, p = 0.044).
Discussion: We assume that 10.5% of mothers who offered exclusively formula milk expressly revoked their desire to breastfeed. However, 25.7% of mothers failed to meet the needs with breast milk, needing to supplement with formula.
Conclusions: Providing Neonatology Units with qualified personnel in this area would improve the breastfeeding rate and consequently, the health of the mother-neonate binomial.
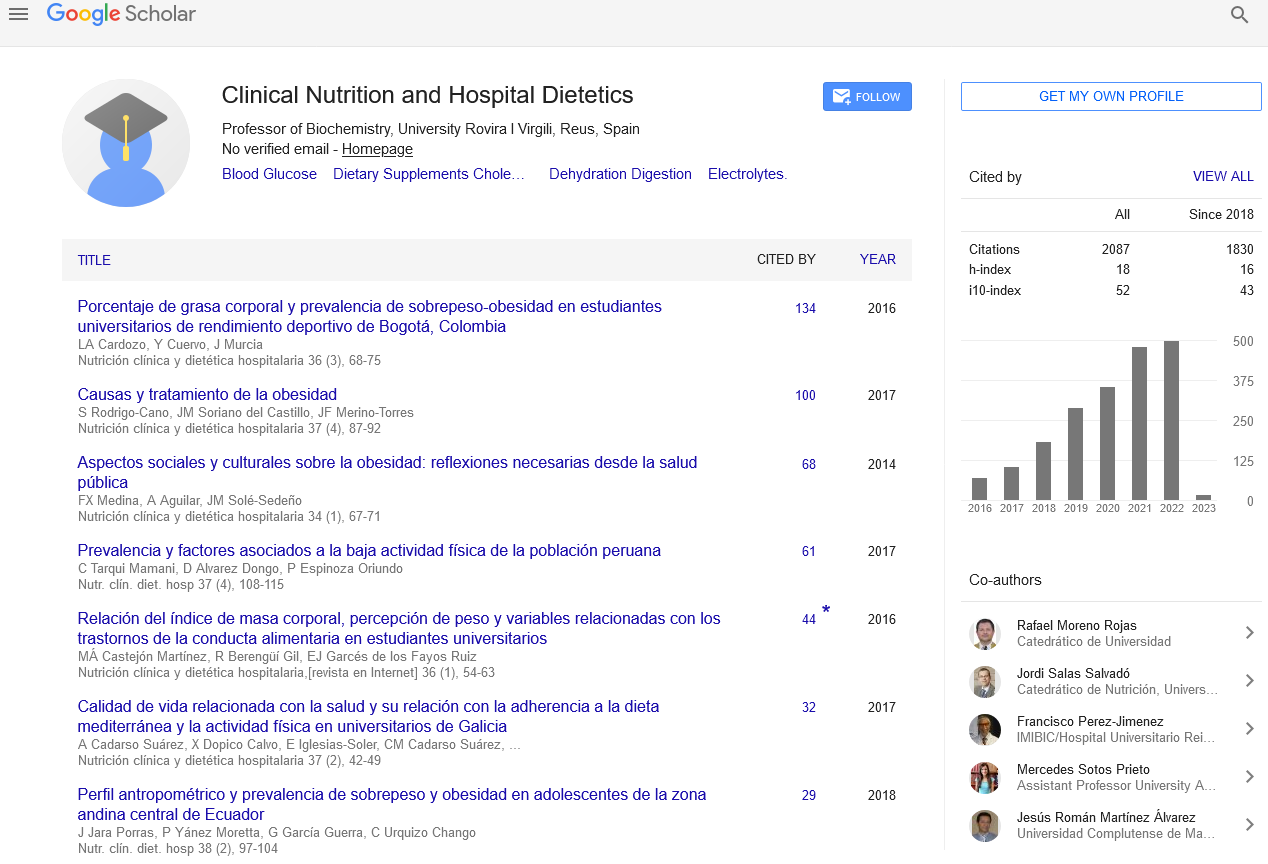
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics