Dietary habits and nutritional status of upper primary school children covered under mid-day meal scheme in rural Punjab
Research Article - (2024) Volume 0, Issue 0
Received: 14-Mar-2024, Manuscript No. CNHD-24-129567; Editor assigned: 18-Mar-2024, Pre QC No. CNHD-24-129567 (PQ); Reviewed: 01-Apr-2024, QC No. CNHD-24-129567; Revised: 08-Apr-2024, Manuscript No. CNHD-24-129567 (R); Published: 15-Apr-2024, DOI: 10.12873/0211-6057.44.S1.003
Abstract
Background and objective: Hardly research has been conducted to investigate how well India’s Mid-Day Meal Scheme (MDMS) ensures that its participants have better dietary habits and optimal nutritional status. The objective of this study was to evaluate the dietary habits and nutritional status of upper primary school children covered under mid-day meal scheme in rural Punjab.
Methods: This cross-sectional research was conducted among 336 adolescent (10-15 years) students of 6th to 8th standard randomly selected from 11 government/ municipality schools selected randomly from the total 112 schools in Khamannon district of rural Punjab in 2018. After taking informed written assent/consent, pretested, semi structured questionnaire was administered. Anthropometric measurements i.e., height, weight were taken to establish malnutrition, underweight, stunting, wasting, overweight and risk of overweight as per World Health Organisation (WHO) guidelines. The data was analysed using SPSS Window Version 17.0 (US).
Results: Out of all the students, 90% liked the MDM which was being served to them. There was 96% regularity in attending the school daily with a slightly less emphasis on the cleanliness maintenance (73%) of the children by the schoolteachers. Malnutrition and underweight were 59% and 50% prevalent, respectively.
The prevalence of stunting was higher in girls (30%). In boys (n=154) both the stunting and wasting was 23%, with 5% and 6% prevalence of overweight and at risk of overweight respectively. Whereas in case of girls (n=182), the prevalence of stunting (30%) was more than wasting (25%) with less girls (3% each) being overweight and at risk of overweight.
Conclusion: Regularity and attendance were up to mark due to increased likeliness of the food by majority of the students, though cleanliness should be improved further. Higher prevalence of malnutrition, wasting and stunting was observed which was even higher among girls. Overweight and risk of overweight was higher among boys. Hence, Nutritional status was unsatisfactory.
Keywords
Dietary habits, Nutritional status, School, Children, Mid-day meal scheme, Punjab
Introduction
Adolescence (10-19 years) age group is a venerable stag of life. As per Erikson, it is the fourth stage of human development, bridging the gap between early school years and young adulthood featuring identity against role confusion [1,2]. A change in body composition, greater physical activity, and rapid linear pubertal growth and development all require an increase in the demands for energy proteins and micronutrients. One of the main determinants of normal pubertal growth timing and pace is adequate nutrition and improved dietary habits [3]. However, as children under five are the most vulnerable group, the majority of health and nutritional surveys and interventions target them, while adolescents are typically ignored [4].
The nutritional status of adolescents enrolled in school is influenced by a wide range of factors, including intrinsic factors like age, gender, order of birth, weight at birth, dietary habits, and medical history, socioeconomic factors like parental education, income, and occupation, and environmental factors like housing location, access to wholesome food and safe water, and environmental hygiene [5-9].
The largest school-based nutritional programme in the world, National Programme for Nutritional Support to Primary Education (NP-NSPE), or Mid-Day Meal Scheme (MDMS) was launched on August 15, 1995, in India, which was late launched on September, 2004 in Punjab [10,11]. In October 2007, plot was additionally stretched out to incorporate the upper primary school children under the Mid-day meal programme with the name changed from National Program of Nutritional Support to Primary Education to National Program of Mid-Day Meal in Schools [12]. The intension was to prevent hunger in the classroom, raise student enrolment and retention rates, strengthen social integration, improve the nutritional state of upper and lower elementary schools (first through eighth standards) and install healthy eating habits [13].
Our present study included the nutritional status and MDM intake of mainly adolescent children as this age group is one of the neglected age groups while they speak to about 16% of the worldwide aggregating around 1.3 billion. With 253 million adolescents, India has the highest adolescent population globally, making up the fifth (about 21%) of the population till 2022 [14]. Poor health and nutrition is one of the primary reasons that adds to the inefficiency of the instructive framework. The expanded dropout rates of malnourished and unhealthy children prompt poor execution in studies. Lacking sustenance in adolescents can possibly hinder improvement and sexual advancement, despite the way that these are likely results of consistent malnutrition in most punctual phases of infancy and adolescence. Insufficient nourishment in teenage years can lay them at great danger of prolonged illnesses especially whenever joined with other adverse way of life practices the issue of malnutrition got acknowledgement of organizers as well as strategy producers ideal from commencement of five-year arranging; a substantial amount of countrywide wholesome projects were executed to battle the hazard of healthy sustenance [15]. Though, lack of healthy sustenance still endures. Therefore, our present study included the children mainly of adolescent age group. The objective was to evaluate the dietary habits and nutritional status of upper primary school children covered under mid-day meal scheme in rural Punjab.
Materials and Methods
This cross-sectional research was conducted among upper primary school children (Class six to eight) from municipality or government schools in Khamanon block, rural Punjab from May to July 2018. Sample size was calculated using Kirkwood and Sterne, 2010 formula: n=4pq/d2, assuming prevalence stunting in the area (p) as 27.4%, q or (1-p) as 72.6%, absolute error (d) as 5% [16,17]. Total sample size was 318. After including 5% nonresponse rate, the final sample size was 336. Eleven (almost 10%) schools were randomly selected from a total of 112 schools form the region. Students were recruited by simple random sampling till the required sample size was obtained. Upper primary class students from 6th to 8th standard from these schools were included for nutritional assessment because 10-15 years age group remains neglected a lot from various child health programmes. Students below the class 6th were excluded from the study. All the study participants were equally taken from the three classes (33.3%).
After taking the informed written assent and consent from the child and parent, respectively; A pretested, semi structured questionnaire was administered. Further the nutritional status of the selected students was assessed by the anthropometric measurements (height and weight) by using the standard equipment. For the measurement of height, an inbuilt stadiometer affixed on the wall was used and for weight, electronic weighting scale was used. Children stood with bare feet on the weighing scale and on the flat ground beside the wall with feet equivalent and with heels, buttocks, shoulders and occiput touching the wall. With the help of a ruler, the topmost point of the head was identified on the wall. The obtained results were then compared with the Anthropometric standards [18]. Body Mass Index (BMI) was calculated using the standard equation: BMI (kg/m2)= Weight (kg)/Height2 (m2). For anthropometric indicators, we followed the WHO growth curves for adolescents. The cut off value for stunting and thinness was <3rd percentile of the WHO standards [19].
Statistical analysis
The data was investigated and reliability drafts were conveyed and entered into the Microsoft Excel. The data was analysed using SPSS Window Version 17.0 (US). Mean (standard deviation) was calculated for continuous variables like height and weight and the prevalence of malnutrition was assessed. The measures of outcome of malnutrition were recorded as” stunting”, “wasting”, “overweight” and “at risk of overweight”. Descriptive analysis was done of the questionnaire for children to analyse the demographic details. All tests of significance were two tailed and level of significance was taken at p-value<0.05.
Results
Demographic profile
The mean age of 336 study participants was 11.7 ± 1.15 years with 32.7% participants belonging to 12-year age group. Out of these total participants, 46% were boys and 54% were girls. All the participants were almost uniformly distributed (approximately 33 percent) within these three classes (Supplementary Table 1).
Dietary patterns of the participants
Around 73% of the participants responded that they eat breakfast before coming to school while 3% of the students responded negatively and 24% responded that they eat breakfast sometimes. Majority of the participants (90%) responded that they eat roti/ chapatti for the breakfast while rice, curry and other type of food was eaten by very few. Almost 33% of the students were getting MDM from 1 year, 33% getting from 2 years and same (33%) of the students were getting MDM from 4 months in this school. Almost all the participants (89%) responded that they liked the Mid-day meal that was served to them during lunch break. Only a small percentage of students (3%) responded negatively while as (7%) replied that they only like the meals sometimes (Table 1).
| Dietary habits of students | ||
|---|---|---|
| Diet preference | Number | Percentage |
| Rice | 7 | 2.08 |
| Roti/chapatti | 303 | 90.18 |
| Curry | 5 | 1.49 |
| Others | 21 | 6.25 |
| Like to eat mid-day meal in school | ||
| Yes | 300 | 89.29 |
| No | 12 | 3.57 |
| Sometimes | 24 | 7.14 |
| Breakfast everyday | ||
| Yes | 244 | 72.62 |
| No | 11 | 3.27 |
| Sometimes | 81 | 24.11 |
| Eating mid-day meal in this school | ||
| 1 year | 113 | 33.63 |
| 2 years | 114 | 33.93 |
| 4 months | 109 | 32.44 |
Table 1. Dietary habits of students covered under Mid-Day Meal Scheme (MDMS)
Anthropometric profile
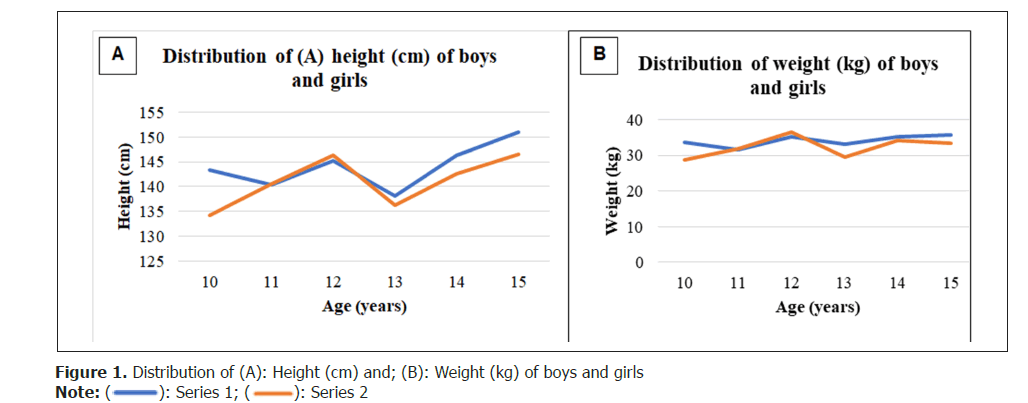
Age specific mean and standard deviation of height, weight and BMI of boys, girls and total participants were calculated and presented in table. Further the difference between the height, weight and BMI of the boys and girls according to the age was depicted through the graph. The mean height of boys (n=154) was 144.10 ± 7.70 cm, girls (n=182) was 141.07 ± 7.46 cm and total participants (n=336) was 142.81 ± 8.48 cm. Boys were taller at age 10, 13, 14 and 15 while the girls were taller than boys at age 12. At the age 11, both the boys and girls were of same height (Table 2 and Figures 1A-1B).
| Height (cm) of the participants | |||||||||
| Age in years | Boys | Girls | Total | ||||||
| N | Mean | S.D. | N | Mean | S.D. | N | Mean | S.D. | |
| 10 | 26 | 143.4 | 8.27 | 6 | 134.3 | 1.79 | 32 | 141.7 | 8.3 |
| 11 | 30 | 140.4 | 8.96 | 76 | 140.53 | 9.26 | 106 | 140.47 | 8.96 |
| 12 | 64 | 145.24 | 9.01 | 46 | 146.3 | 8.16 | 110 | 145.6 | 9.01 |
| 13 | 25 | 138.2 | 11.6 | 41 | 136.2 | 11.8 | 66 | 136.9 | 11.6 |
| 14 | 8 | 146.4 | 8.4 | 11 | 142.6 | 8.3 | 19 | 144.2 | 8.05 |
| 15 | 1 | 151 | 0 | 2 | 146.5 | 5.5 | 3 | 148 | 4.96 |
| Total | 154 | 144.1 | 7.7 | 182 | 141.07 | 7.46 | 336 | 142.81 | 8.48 |
| Weight (Kg) of the participants | |||||||||
| Age in years | Boys | Girls | Total | ||||||
| N | Mean | S.D. | N | Mean | S.D. | N | Mean | S.D. | |
| 10 | 26 | 33.63 | 7.63 | 6 | 28.65 | 4.49 | 32 | 32.7 | 7.41 |
| 11 | 30 | 31.56 | 7.38 | 76 | 31.77 | 7.43 | 106 | 31.56 | 7.38 |
| 12 | 64 | 35.22 | 10.37 | 46 | 36.47 | 10.89 | 110 | 35.74 | 10.37 |
| 13 | 25 | 33.03 | 7.19 | 41 | 29.58 | 7.34 | 66 | 30.89 | 7.19 |
| 14 | 8 | 35.33 | 4.94 | 11 | 34.16 | 4.93 | 19 | 34.65 | 4.81 |
| 15 | 1 | 35.8 | 3.25 | 2 | 33.3 | 3.8 | 3 | 34.13 | 3.31 |
| Total | 154 | 34.09 | 6.25 | 182 | 32.32 | 6.48 | 336 | 33.27 | 6.74 |
Table 2. Distribution of height (cm) and weight (kg) of study participants
The mean BMI of boys (n=154) was 16.34 ± 2.27, girls (n=182) was 16.19 ± 2.39 and total parti- - -cipants (n=336) was 16.20 ± 2.35. Same trend was fo- -und in the BMI as that of height and weight with the exception at age 14, where girls were thinner as comp- -ared to boys. (Table 3) (Figure 2)
| Age in years | Boys | Girls | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean | S.D. | N | Mean | S.D. | N | Mean | S.D. | |
| 10 | 26 | 16.2 | 2.72 | 6 | 15.91 | 2.75 | 32 | 16.14 | 2.73 |
| 11 | 30 | 15.88 | 2.74 | 76 | 15.81 | 2.83 | 106 | 15.88 | 2.74 |
| 12 | 64 | 16.46 | 3.4 | 46 | 16.79 | 3.58 | 110 | 16.64 | 3.4 |
| 13 | 25 | 17.34 | 3.32 | 41 | 16.5 | 3.4 | 66 | 16.46 | 3.32 |
| 14 | 8 | 16.48 | 1.44 | 11 | 16.69 | 1.21 | 19 | 16.6 | 1.41 |
| 15 | 1 | 15.7 | 0 | 2 | 15.44 | 0.6 | 3 | 15.53 | 0.51 |
| Total | 154 | 16.34 | 2.27 | 182 | 16.19 | 2.39 | 336 | 16.2 | 2.35 |
Table 3. BMI of study participants
Prevalence of malnutrition
The overall prevalence of malnutrition among the study participants in the present study was found to be 59%. The overall prevalence of underweight was found to be 50% while that of overweight was very low (4%) with 5% of the students were at the risk of being overweight.
Stunting
Prevalence of stunting was calculated by comparing height-for-age with the WHO standards which was great- er among girls (30%) than their male equivalents (23%) (Figures 3A-3B).
Thinness (wasting), overweight and risk of overweight
Prevalence of thinness, overweight and at the risk of be- ing overweight was calculated by comparing the BMI-for- age with the WHO standards. When the prevalence of thinness was evaluated, girls (25%) were slightly more affected as compared to boys (23%). Similarly for the prevalence of overweight or at the risk of overweight, boys (5%, 6% respectively) were slightly more affected than girls (3%,3%) (Figures 3C-3D).
Discussion
Mid-Day Meal Scheme (MDMS) was executed by Government of India to build enrolment of schools, to remove the social inequalities and to combat the problem of malnutrition. In the present study, school going children (10-15 years) were enrolled. This was under adolescent age group. Great sustenance and decent nourishment is fundamental for survival, bodily development, psychological improvement, execution and profitability, prosperity as well as welfare of these children [20].
In the present study it was found that 73% of the students eat breakfast before coming to school regularly which was much higher as compared to the report on MDMS in Telangana which was only 10% [21]. Absence of satisfactory breakfast over expanded timeframe can fundamentally influence the dietary status of the children. Similar results were found from the study conducted in the two districts of Punjab where the breakfast intake was 60% [22]. In Gujarat, the breakfast intake was 90%- 100% among the school children [23]. According to the present study, the cooked Mid-day meal was enjoyed by 73% of the students in comparison to 84% in Andhra Pradesh [24]. Other studies described much higher percentage of Mid-day meal being liked by the students [21,22]. Ninety-six percent regularity in attendance was found in the present study. Increased attendance and enrolment of the schools was found from the introduction of mid- day meal [9-13]. Almost three-fourth (74%) of the students were checked for cleanliness regularly and all the students were covered for the health checkup and iron and folic acid as well as deworming tablets [25-29]. Same results as the present study were found from the mid-day meal review of Gujarat [23]. In contrast, all the schools were not regularly checked up by the health professionals as well as Iron Folic Acid (IFA) and deworming (Albendazole) tablets were given only to 29% of the students [21]. There is an urgent need to take action for the correct execution of school wellbeing health program with the goal that children could get IFA and deworming tablets [30].
The chief outcome of the existing study, the prevalence of malnutrition (59%) was found to be higher. Half of the (50%) adolescents were undernourished and 4% were over nourished. The risk of overweight was observed to be 5%. The estimated prevalence of undernutrition (50%) was high (21%) as compared to a report of joint survey mission on Mid-day meal in Districts Roopnagar and Jallandhar of Punjab while the overweight status was almost same (4%) [22].
Relatively higher (64%) under nutrition prevalence was reported by the same joint review report of the nutritional status of school children in Telangana [21]. Severe under nutrition of about 90% was reported from a study on the tribal children of West Bengal provided with Mid- day meal [31]. Stunting is the consequence of long-term deficiency of nutritious content and the predictable prevalence of stunting in this study was 26.5% (23% boys, 30% girls). This evaluation was approximately alike to the amount of stunting amongst school children by a report on Mid-day meal Gujarat [23]. This result yielded the insufficiencies of the current structure to deal with under nutrition. A greater predominance of stunting has been recently announced from India. The given account of local WHO consultation on dietary status of adolescent girls revealed 45% pervasiveness of stunting among girls and 20% among boys with an average of 32% in both genders [32].
In our examination, mean height of girls was lower than the boys at age (years) 11, 13 and 15 but the girls were taller at age 12 and were of the same height as that of boys at age 11, most likely due to the early beginning of adolescence in girls. Similarly, the boys were taller after age 13 to age 15, due to the pubertal onset in boys. A comparative finding has been accounted from the Wardha district [33]. When the prevalence of thinness was assessed, girls (25%) were more influenced than boys (23%). On the contrary, boys were more influenced than girls (59.4% versus 41.3%) during adolescence [34].
The prevalence of thinness (24% total: 23% boys, 25% girls) was very high in the study compared to the National Nutrition Monitoring Bureau (NNMB) report (9%) [35]. A study conducted in the rural area of Tripura reported a much higher prevalence of thinness among the children aged 10-15 years [36]. Forty-five percent of severe thinness was found among the boys and girls equally in the tribal schools of Gujarat [37]. Similar higher prevalence of thinness was also reported from a study conducted in two districts of India [38].
Thinness was more prevalent during this age group gather on account of the development spurt and sudden increment in stature of the adolescents. The study conducted by de Onis, et al. in West Bengal on adolescents, it was found that the prevalence of thinness was about 5 times (50%) that of stunting (11%) [39]. Regardless of the gender, the prevalence of stunting and wasting (25.5%- 51%, 42%-75.4% respectively) was higher according to a study conducted in rural schools of south India [40]. Similarly, there was a very high commonness of under nutrition among provincial adolescents of Darjeeling as the prevalence of stunting and thinness was found to be 46.6% and 42.4% respectively [41].
The strength of our study was to unleash the ground level facts and to unveil the curtain from the scarcity of studies depicting the development of adolescents in view of the challenges in translating anthropometric information in this age gathering especially in rural Punjab. Inability to establish temporality and causation was the most important limitation. Others were the presence of recall bias, social disability bias and residual confounding. This study could not be generalisable due to recruitment only from rural population.
Conclusion
Overall, this research revealed the impact of MDMS on the dietary habits and nutritional status of the upper primary school students in rural Punjab. Due to increased likeliness of the food by majority of the students, regularity and attendance were up to mark, though cleanliness should be improved. Higher prevalence of malnutrition, wasting and stunting was observed which was even higher among girls. Overweight and risk of overweight was higher among boys. Hence, Nutritional status was unsatisfactory. Evidence based trials with multiple follow ups and continuous nutritional surveillance across the nation are recommended to draw proper implementation steps.
Declaration
Ethical approval and consent to participant
In present study, ethical clearance was taken from PGIMER intramural ethical committee for the initiation of the study (NK/4434/MPH). All the ethical criteria were fulfilled before, at the time and after the data collection as per Helsinki declaration. Permission to conduct this research study in schools of district Fatehgarh Sahib (MDMS/GM/2018/8014) was taken from the Deputy State Project Director, Mid-Day Meal Society, Mohali, Punjab.
Consent for publication
All authors have provided consent for publication.
Availability for supporting data
Any other queries can be emailed to the corresponding author.
Conflict of interests
Authors declare no competing interest.
Funding
None
Author’s contributions
Conceptualization: PK and TS; data curation, HK and RS; Formal Analysis, HK and PH; Resources, TS and PK; Methodology, PK and RS; Software, HK and PH; Supervision, PK; Investigation and Project administration, PK and TS; Visualization, PK and HK; Roles/writing-original draft: HK and PH and writing -review and editing; PK and RS.
References
- Eccles JS. The development of children ages 6 to 14. Future Child. 1999;9(20):30-44.
[Crossref] [Google Scholar] [Indexed]
- Kliegman RM, Behrman RE, Jenson HB, Stanton BM. Nelson textbook of pediatrics e-book. Elsevier health sci. 2007.
- Soliman A, Alaaraj N, Hamed N, Alyafei F, Ahmed S, Shaat M, et al. Review nutritional interventions during adolescence and their possible effects. Acta Biomed. 2022; 93(1).
[Crossref] [Google Scholar] [Indexed]
- Daboné C, Delisle HF, Receveur O. Poor nutritional status of schoolchildren in urban and peri-urban areas of Ouagadougou (Burkina Faso). Nutr J. 2011; 10:1-8.
[Crossref] [Google Scholar] [Indexed]
- Assefa H, Belachew T, Negash L. Socio-demographic factors associated with underweight and stunting among adolescents in Ethiopia. Pan Afr Med J. 2015;20.
[Crossref] [Google Scholar] [Indexed]
- Saito K, Korzenik JR, Jekel JF, Bhattacharji S. A case-control study of maternal knowledge of malnutrition and health-care-seeking attitudes in rural South India. Yale J biol med. 1997;70(2):149.
- Nutrition in Middle Childhood and Adolescence. United Nat Child Fund. 2004
- Von Laer Tschudin L, Chattopadhyay C, Pandit S, Schramm-Garaj K, Seth U, Debnath PK, et al. Risk factors for under-and overweight in school children of a low income area in Kolkata, India. Clin Nutr. 2009;28(5):538-542.
- Ao M, Lhungdim H. Re-estimating malnourishment and inequality among children in North-East India. Econ pol Week. 2014:53-63.
- Mid-day meal. Educ Depart Delhi.2013
- Chutani AM. School lunch program in India: Background, objectives and components. Asia Pac J Clin Nutr. 2012;21(1):151-154.
- Prasad HA, Sinha NK, Khan RA. Performance of major social sector schemes: A sample survey report. 2014.
- Kainth GS. Diagnostic analysis of mid day meal programme in rural Punjab. Academia Edu. 2013.
- Adolescent: Investing in a safe, healthy and productive transition from childhood to adulthood is critical. UNICEF data. 2024
- Naigulevu A. Ghai essential paediatrics. Academia. 2023.
- Kirkwood BR, Sterne JA. Essential medical statistics. John Wiley Sons. 2010.
- Pandurangi R, Mummadi MK, Challa S, Reddy NS, Kaliaperumal V, Hemalatha R. Burden and predictors of malnutrition among Indian adolescents (10-19 years): Insights from comprehensive national nutrition survey data. Front Public Heal. 2022;10:877073
- Dietary Guidelines for Indians. Indian Coun Med Res.2018
- Brook, Darville CG. Growth assessment in childhood and adolescence. World Health Organ. 1982:164.
- Berger LM, Font SA. The role of the family and family-centered programs and policies. Future Child. 2015;25(1):155.
- Report of 7th Joint review mission mid day meal scheme Telangana. Ministry Hum Resour Dev. 2015.
- Report of 10th Joint review Mission on mid-day meal scheme Punjab. Ministry Hum Resour Dev. 2018.
- Report of 10th Joint review mission mid-day meal scheme Gujarat. Ministry Hum Resour Dev. 2018.
- Pinisetty R. Community participation in mid-day meal scheme: Exclusion and inclusion in Andhra Pradesh. Sch Res J Int Stud. 2015;3(19):662-670.
- Dreze J, Goyal A. Future of mid-day meals. Econ Pol Week. 2003;38(44):4673-4683.
- Khera R. Mid-day meals in primary scho ols: Achievements and challenges. Econ pol weekly. 2006:4742-4750.
- Laxmaiah A, Rameshwar Sarma KV, Rao DH, Reddy G, Ravindranath M, Rao MV, et al. Impact of mid day meal program on educational and nutritional status of school children in Karnataka. Indian Pediatr. 1999;36(12):1221-1228.
- Rajan SI, Jayakumar A. Impact of noon meal programme on primary education: An exploratory study in Tamil Nadu. Econ Pol Week. 1992:27(43);2372-2380.
- Alderman H, Bundy D. School feeding programs and development: Are we framing the question correctly?. World Bank Res Obser. 2012; 27(2):204-221.
- Report of 10th Joint review mission on mid-day meal scheme Arunachal Pradesh. Ministry Hum Resour Dev. 2017.
- Mittal PC, Srivastava S. Diet, nutritional status and food related traditions of Oraon tribes of New Mal (West Bengal), India. Rural Remote Health. 2006;6(2):1-11.
- Mental health of adolescents. World Health Organ.1998.
- Rao NP, Singh D, Krishna TP, Nayar S. Health and nutritional status of rural primary school children. Indian Pediatr. 1984;21(10):777-783.
- Medhi GK, Hazarika NC, Mahanta J. Nutritional status of adolescents among tea garden workers. Indian J Pediatr. 2007;74:343-347.
- Diet and nutritional status of rural population, prevalence of hypertension and diabetes among adults and infant and young child feeding practices. Indian Coun Med Res. 2012
- Uddin MJ, Nag SK, Sil SK. Anthropometric assessment of nutritional status of adolescents in rural school of Unokoti district of Tripura, North-East India. Anthropolog. 2015;19(1):277-284.
- Nambiar VS, Roy K, Patel N, Saha C. Vitamin A deficiency and anemia: Alarming public health problems among the tribal Rathwa adolescents of Chhota Udaipur, Gujarat, Western India: A cross-sectional study. Int J Med Sci Public Health. 2015;4(11):1-9. [Crossref]
- Mitra A, Rao N. Gender differences in adolescent nutrition: Evidence from two Indian districts. LANSA Work Paper. 2017;2017:13.
- de Onis M, Dasgupta P, Saha S, Sengupta D, Blössner M. The national center for health statistics reference and the growth of Indian adolescent boys. Am J Clin Nutr. 2001;74(2):248-253.
[Crossref] [Google Scholar] [Indexed]
- Haboubi GJ, Shaikh RB. A comparison of the nutritional status of adolescents from selected schools of South India and UAE: A cross-sectional study. Indian J Community Med. 2009;34(2):108-111.
[Crossref] [Google Scholar] [Indexed]
- Mondal N, Sen J. Prevalence of stunting and thinness among rural adolescents of Darjeeling district, West Bengal, India. Italian J Pub Heal. 2010;7(1).
Author Info
Harpreet KAUR1, Pritam HALDER2, Rachana SRIVASTAVA2, Tarundeep SINGH2 and Poonam KHANNA2*2Department of Community Medicine and School of Public Health, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics