Frequent consumption of savory snacks is associated with NAFLD in Indian adult population: A case control study
Research Article - (2023) Volume 43, Issue 2
Received: 10-Jul-2023, Manuscript No. CNHD-23-105360; Editor assigned: 12-Jul-2023, Pre QC No. CNHD-23-105360 (PQ); Reviewed: 26-Jul-2023, QC No. CNHD-23-105360; Revised: 02-Aug-2023, Manuscript No. CNHD-23-105360 (R); Published: 09-Aug-2023, DOI: 10.12873/0211-6057.43.02.200
Abstract
Introduction: Non-Alcoholic Fatty Liver Disease (NAFLD) has emerged as a public health problem in India against the backdrop of diabetes, dyslipidemias, and central obesity. It is related to lifestyle factors including diet and physical activity.
Aim: To study the association between lifestyle factors and NAFLD, in an adult Indian population.
Materials and Methods: The study included 320 subjects, comprising 160 cases (patients with NAFLD) and 160 controls (without NAFLD), and were recruited from a tertiary care hospital in North India. Data on socio-demographic profile, clinical, and anthropometric parameters, biochemical measurements, dietary pattern and physical activity patterns were obtained.
Results: Risk factors for NAFLD included central obesity (waist circumference >80 cm in females and >90 cm in males), high consumption of edible oil (>25 g for males and >20 g for females), evening snack intake, intake of savory intake more than twice a week, intake of alcohol (even less than the cut-off).
Conclusion: The lifestyle risk factors of the present study can be incorporated as components of nutrition and lifestyle education programs on preventive strategies for NAFLD at both clinical and community level.
Keywords
NAFLD, Evening snacks, Savory snacks, Food frequency questionnaire, Lifestyle risk factors, Edible oil.
Abbreviations
DM: Diabetes Mellitus; CVD: Cardiovascular Disorders; HT: Hypertension WHR: Waist-to-Hip Ratio; WHtR: Waist-to-Height Ratio; BP: Blood Pressure; PP: Postprandial; HDL-C: High-Density Lipoprotein Cholesterol; LDL-C: Low-Density Lipoprotein Cholesterol; VLDL-C: Very Low-Density Lipoprotein Cholesterol; SGOT: Serum Glutamic Oxaloacetic Transaminase; SGPT: Serum Glutamic Pyruvic Transaminase.
Introduction
Non-Alcoholic Fatty Liver Disease (NAFLD) has emerged as one of the most common chronic liver diseases globally. It includes a histological spectrum of diseases, such as Non-Alcoholic Fatty Liver (NAFL), Non-Alcoholic Steatohepatitis (NASH), advanced fibrosis, cirrhosis, and hepatocellular carcinoma in the absence of alcohol intake [1]. The progression of NAFLD is associated with lifestyle factors mainly improper diets and lower physical activity and is mainly due to modernization and urbanization across the globe.
Studies have suggested the associations of NAFLD with obesity, abdominal obesity, components of metabolic syndrome, improper quality of food (high intake of total fats, higher intake of saturated fats and n6 Polyunsaturated Fatty Acid (PUFA) along with simple carbohydrate content, low physical activity, and genetic background [2]. Other lifestyle factors like snacks and alcohol intake along with smoking are also shown to have an association with NAFLD [3,4]. All these may be risk factors for diabetes, cardiac health, and overall mortality [5]. The Ministry of Health and Family Welfare in India highlighted the need for a holistic approach along with the integration of public health measures to prevent NAFLD into the existing national program for Non-Communicable Diseases (NCDs)-the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS) [6].
Therefore, the present study was undertaken to study the relationship between lifestyle risk factors, and NAFLD in an Indian population.
Case Presentation
Subjects
The study included 320 subjects, comprising 160 cases (patients with NAFLD) and 160 controls (without NAFLD), and were enrolled from the Gastroenterology & Medicine OPDs at All India Institute of Medical Sciences (AIIMS), New Delhi, India.
Study design
This observational case-control study was conducted in All India Institute of Medical Sciences, New Delhi, a tertiary care hospital in India. Adults of both genders (18 to 60 years) who fulfilled the inclusion criteria for either cases or controls were enrolled in the study.
Eligibility criteria for cases
• Fatty liver on radiological examination (ultrasound) in the previous month
By interview-cum-questionnaire method that the current/ recent alcohol consumption is less than 21 drinks on average per week in males and less than 14 drinks on average in females per week [7].
Eligibility criteria for controls
• Healthy volunteers with no diagnosed fatty liver on radiological examination (ultrasound) in the previous month
Alcohol consumption of fewer than 21 drinks on average per week in males and less than 14 drinks on average in females per week [8].
Exclusion criteria for both cases and controls
• History of Chronic Liver Disease (CLD)
• History of intake of drugs leading to fatty liver like steroids, tetracycline, tamoxifen, valproic acid, oral contraceptives, or corticosteroids
• Patients with chronic diseases like Type 2 Diabetes, Cardiovascular Disease (CVD), Inflammatory Bowel Disease (IBD), Human Immune Deficiency Infection (HIV) and pregnant and lactating women
• Patients with presence of Hepatitis B surface Antigen (HBs Ag),anti-HCV antibody (antibody to hepatitis C virus) and anti-HIV antibody (anti-HIV)
• Patients enrolled in any kind of weight loss intervention.
A pretested and standardized questionnaire cum interview schedule was used to collect information on age, gender, family profile, and socioeconomic status. Anthropometric measurements were undertaken using standard WHO techniques [9]. Height: The height was measured to the nearest 0.1 cm using a stadiometer. Weight: Weight was measured to the nearest 100 grams using an electronic scale (Seca Model 803). Waist circumference (WC) and hip circumference were measured to the nearest 0.1 cm. The waist circumference and hip circumference were measured at a level midway between the lowest rib and the iliac crest and the level of the great trochanter, respectively. Body Mass Index (BMI): (Weight in kilograms divided by the square of height in meters) was calculated by Quetelet’s ratio. BMI and Waist-to-Hip Ratio (WHR) cut-offs as per the Asian Indian population were used [10].
Clinical parameters included blood pressure measurements. Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) were recorded in a sitting position. An average of three readings was noted after a gap of 5 minutes using an automated blood pressure instrument (Omron HEM-7203, Kyoto, Japan). Biochemical parameters for cases and controls were undertaken after 10-12 hours of overnight fasting at the AIIMS laboratory using standard laboratory procedures. Trans abdominal ultrasonography of the liver was performed using a 1-5 MHz curvilinear transducer (iU22, Philips, Netherlands) by the same trained radiologist for all participants after an overnight fast. For the Fibroscan test, LSM (measured in kilopascals (kPa) and CAP score measurements (to find steatosis grade (S0,S1,S2), were measured in decibels per meter (dB/m), were undertaken with Echosens-Fibroscan Touch 502 Model (2015), with subjects in supine position with around 3 hours of fasting. A valid LSM was defined as the median value of 10 acquisitions, given an interquartile range divided by the median (IQR/M) of ≤ 30%. CAP was reported in dB/m, using the median of 10 acquisitions. The Interquartile Range (IQR) was registered for all measurements [11].
Dietary intake was measured by a 24-hour recall method for 2 days and by Food Frequency Questionnaire (FFQ) method in which foods consumed in the last year was reported by patients. Questions on snacking pattern and frequency of savoury snacks consumed during evening time was asked with the list of savory snacks like packed namkeen, matthi, samosa etc. i.e. foods which are prepared using high quantity of oil and salt. Physical Activity Pattern was analyzed by the Global Physical Activity Questionnaire (GPAQ) Version 2 [12].
Sample size
In the absence of the prevalence of various risk factors and their associated odds ratio, no formal sample size calculation could be performed, based on a literature search about 16 risk factors emerged, thus about 10 cases per potential risk factor were enrolled. Therefore, 160 cases and 160 controls were enrolled in the study, giving a total sample size of 320. The level of confidence was 95% and a power of 80% was taken [13].
Statistical analysis
Data were analyzed with help of the statistical software STATA 14.0. Qualitative data were expressed as frequency and percentage, quantitative data as Means ± SD and Median (Inter quartile). Levels of significance less than <0.05 was described as significant. Independent t-test and Mann-Whitney U test were used to compare the quantitative variable between the groups. Bivariate analysis was performed using the chi-square test (Fischer exact test, wherever applicable). For bivariate analysis, Waist Circumference (WC), Waist-to-Hip Ratio (WHR), Waist-to-Height Ratio (WHtR), glycemic, lipid profile, and high blood pressure, were categorized according to standard guidelines. As values for WC, WHR and WHtR were highly correlated (the latter two are calculated from the former), only waist circumference was included in the regression equation. Those variables which were found statistically significant in univariate analysis and were clinically meaningful with p-value <0.1 were included in the multivariable logistic regression model. Stepwise logistic regression was undertaken in the multivariable regression analysis to identify the independent risk factors of NAFLD. Multinomial logistic regression was conducted to analyze the association between liver steatosis (CAP score) and anthropometric parameters.
Results
In this study, 70% of the subjects in both groups belonged to nuclear families. Socio-Economic Status (SES) as a composite value was calculated on basis of income, education, and occupational status of the subjects [14]. A higher number of cases compared to controls had a positive and significant family history of diabetes (p<0.05) (Table 1).
| Variable | Cases (n=160) n(%) | Controls (n=160) n(%) | p-value |
|---|---|---|---|
| Age | |||
| 18-30 years | 23(14.37) | 23(14.37) | |
| 30-45 years | 93(58.12) | 99(61.87) | 0.731 |
| 45-60 years | 44(27.5) | 38(23.75) | |
| Gender | |||
| Male | 80(50) | 80(50) | |
| Female | 80(50) | 80(50) | 0.999 |
| Family | |||
| Joint | 45(28.13) | 47(29.38) | |
| Nuclear | 115(71.88) | 113(70.63) | 0.805 |
| Socioeconomic Status | |||
| Upper Lower (IV) | 05(3.1) | 14(8.75) | |
| Lower Middle (III) | 20(12.5) | 26(16.25) | 0.005 |
| Upper Middle (II) | 117(73.1) | 115(71.8 | |
| Upper(I) | 18(8.7) | 5(3.1) | |
| Family history | |||
| Parent DM | 44(27.50) | 27(16.88) | 0.022 |
| Parent CVD | 21(13.13) | 22(13.75) | 0.87 |
| Parent Liver Disease | 5(3.13) | 4(2.50) | 0.735 |
| Parent HT | 44(27.50) | 41(25.62) | 0.704 |
Categorical variables are presented as n (%). P-value was determined by the chi-square test/Fisher’s exact t-test. All bold styling expressions are statistically significant (p<0.05).
The average age of NAFLD cases was 39.8 ± 8.4 years and was 39.43 ± 8.6 years in controls. The mean age and BMI of cases and controls were comparable. Among the NAFLD cases vs. controls, the BMI of 18-22.9 (normal) was 11.88% vs. 13.75%; the BMI of 23-24.9 (overweight) was 18.75% vs. 18.13% and BMI >25 (obese) was 69.38% vs. 68.13%. Patients with NAFLD had significantly higher values of waist circumference, waist-to- hip ratio, waist-to-height ratio, systolic blood pressure, and diastolic blood pressure (p<0.05). The biochemical parameters namely fasting and postprandial glucose, triglycerides, total cholesterol, LDL cholesterol, VLDL cholesterol, SGOT, and SGPT were significantly higher in NAFLD cases versus controls (p<0.05) (Table 2).
| Variable | NAFLD Cases (n=160) Mean ± SD | Controls(n=160) Mean ±SD | p-value | ||
|---|---|---|---|---|---|
| Age (Years) | 39.8 ± 8.4 | 39.4 ± 8.6 | 0.699 | ||
| BMI (kg/m) | 26.9 ± 3.4 | 26.8 ± 3.6 | 0.809 | ||
| Waist Circumference (cm) | |||||
| Male | 90.91 ± 7.36 (65.5-112.0) | 84.91 ± 6.43(72-106) | <0.001 | ||
| Female | 82.23 ± 8.14 (64-102) | 77.18 ± 7.26(52-93) | <0.001 | ||
| WHR | |||||
| Male | 0.91 ± 0.05(0.77-1.08) | 0.89 ± 0.04(0.81-0.98) | 0.001 | ||
| Female | 0.80 ± 0.09(0.68-1.3) | 0.77 ± 0.05(0.64-0.9) | 0.011 | ||
| WHtR | |||||
| Males | 0.54 ± 0.04(0.39-0.66) | 0.51 ± 0.044(0.38-0.65) | <0.001 | ||
| Female | 0.52 ± 0.05(0.38-0.67) | 0.50 ± 0.0.04(0.36-0.63) | <0.001 | ||
| Systolic BP (mm Hg) | |||||
| Male | 129.3 ± 10.3(104-166) | 121.3 ± 3.6(112-137.5) | <0.001 | ||
| Female | 124.7 ± 5.8(110-138) | 116.5 ± 6.7(98-128) | <0.001 | ||
| Diastolic BP (mm Hg) | |||||
| Male | 81.6 ± 6.5(63-104) | 80.1 ± 4.4(56.5-97) | <0.001 | ||
| Female | 81.3 ± 2.8(70.5-86) | 76.6 ± 5.8(62-85) | 0.001 | ||
| Fasting blood glucose (mg/dl) | |||||
| Male | 94.77 ± 9.62(67-124) | 91.11 ± 7.82(78-115) | 0.004 | ||
| Female | 95.19 ± 10.58(72-130) | 89.86 ± 9.58(62-109) | 0.005 | ||
| Postprandial (mg/dl) | |||||
| Male | 110.53 ± 28.29(60-191) | 101.23 ± 28.2(43-178) | 0.035 | ||
| Female | 113.91 ± 23.43(74-191) | 100.25 ± 22.52(50-171) | <0.001 | ||
| Triglycerides * (mg/dl) | |||||
| Male | 146(111.5-200) | 119(75-159)* | 0.001 | ||
| Female | 110(76.5—149.5) | 96 (73-120.5) | 0.108 | ||
| Total cholesterol (mg/dl) | |||||
| Male | 190.08 ± 42.61(81-322) | 163.61 ± 37.51(80-263) | <0.001 | ||
| Female | 190.37 ± 38.93(108-313) | 179.47 ± 37.53(108-311) | 0.082 | ||
| HDL-C (mg/dl) | |||||
| Male | 40.83 ± 6.17(20-55) | 40.15 ± 7.6(22-57) | 0.335 | ||
| Female | 46.1 ± 7.34(28-62) | 44.12 ± 8.12(22-58) | 0.113 | ||
| LDL-C (mg/dl) | |||||
| Male | 119.85 ± 33.72(45-215) | 103.50 ± 32.2(43-194) | 0.001 | ||
| Female | 124.80 ± 31.51(61-215) | 117.22 ± 32.27(63-231) | 0.158 | ||
| VLDL-C *(mg/dl) | |||||
| Male | 26(19-39) | 17(13-24.5) | <0.001 | ||
| Female | 19(13-25) | 17(11.5-22) | 0.206 | ||
| SGOT (IU/L) | |||||
| Male | 32.56 ± 11.38(16-72) | 28.20 ± 16.06(5.6-43) | <0.001 | ||
| Female | 23.55 ± 8.05(13-73) | 22.61 ± 6.42(11-42) | 0.544 | ||
| SGPT (IU/L) | |||||
| Male | 40.5 (30-53.5) | 27 (20-43.5) | <0.001 | ||
| Female | 20 (16-28) | 19.5 (16-25) | 0.392 | ||
| Alcohol intake | |||||
| No | 127 (79.3) | 142 (88.7) | |||
| Yes | 33 (20.6) | 18 (11.2) | 0.022 | ||
| Smoking | |||||
| No | 141 (88.13) | 148 (92.5) | |||
| Yes | 19 (11.88) | 12 (7.5) | 0.186 | ||
| CAP Score (db/m) | 266.5 ± 59.4 (100-375) | 215.8 ± 53.8 (100-367) | <0.001 | ||
| Liver Stiffness Measurement (LSM) (kPa) | 5.1 ± 1.8 (2.4-13.8) | 4.5 ± 1.5(2.2-9.7) | <0.001 | ||
Note: Independent t-test applied. All bold styling expressions are statistically significant (p<0.05).
*: Represents data as Median (IQR) and Wilcoxon Rank sum test applied. Figures in parentheses.
Odds ratios (OR) and their 95% confidence interval of the associations between modifiable lifestyle risk factors and NAFLD are presented in Table 3. For NAFLD patients, it was observed that known risk factors like increased waist circumference, low physical activity, a positive family history of diabetes along with higher quantity of edible oil (more than 25 g for males and more than 20 g for females) (OR 2.2; 0.96-4.97, p=0.040), intake of evening snack (OR 2.1;1.18-3.97,p=0.012),intake of evening savory snacks more than twice/week (OR 2.7(1.33-3.23), intake of alcohol (even less than the cut-off) (OR 2.7; 1.30-5.62, p=0.008), are the major factors associated with NAFLD.
| Variable | Cases (160) n (%) | Control (160) n (%) | p-value | OR (95 % CI) | p-value |
|---|---|---|---|---|---|
| Edible oil (g) as per dietary guidelines | |||||
| < 25 g males, <20 g females |
15(9.3) | 29(18.1) | 1 | ||
| > 25 g males, >20 g females |
145(91.8) | 131(81.9) | 0.02 | 2.5(1.24-5.01) | 0.01 |
| Evening snacks intake | |||||
| No | 27(16.8) | 48(30.0) | 1 | ||
| Yes | 133(83.1) | 112(70.0) | 0.02 | 2.1(1.23-3.60) | 0.01 |
| Frequency of savory snacks | |||||
| Frequency≤2/week | 42 (26.2) | 63(39.3) | 0.01 | 1 | |
| Frequency>2/week | 118 (73.8) | 97 (60.7) | 2.7(1.33-3.23) | 0.02 | |
| Alcohol intake | |||||
| No | 127(79.3) | 142(88.7) | 1 | ||
| Yes | 33(20.6) | 18(11.2) | 0.02 | 2.0(1.10-3.81) | 0.02 |
Discussion
The present study was carried out to study the association of lifestyle risk factors with NAFLD. The biochemical parameters (lipid profile) showed significant differences in cases versus controls in males but not in females. Some studies state that various gender-specific mechanisms, like the effect of sex hormones and differences in lifestyles and physiology, influence the prevalence of NAFLD. Several studies reported NAFLD as being more frequently detected in males than females. However, studies from Western and Asian populations, suggest that NAFLD is generally more common in females [15]. Understanding the association between NAFLD and gender differences will facilitate focusing on specific groups to improvise health and prevent disease. It will also provide treatment strategies to decrease the rates of morbidity and mortality associated with NAFLD and its associated pathologies [16].
According to the findings of the present study, central obesity (WC, WHR, and WHtR) revealed a higher magnitude of risk for males as compared to females of the NAFLD group. Studies from India have reported waist circumference as an independent predictor of NAFLD [16-19]. Waist circumference is an indicator of the accumulation of abdominal fat. Waist circumference is a simple and accessible index to detect the increased risk of steatosis and can be used in clinical settings for screening NAFLD patients [16].
Another risk factor for fatty liver in the present study was low physical activity previously reported study on NAFLD patients had low physical activity and were sedentary versus healthy controls [20,21]. A low level of physical activity was also reported in NAFLD subjects; however, it was not a significant predictor [20]. Another study revealed that low physical activity was not associated with NAFLD though the resting time was higher in NAFLD subjects versus the subjects without NAFLD [22].
The quantity of dietary fat may have a direct impact on the fat content of the liver, and high-fat diets are harmful [23]. Higher intake of edible oil compared to the dietary guidelines was an important risk factor for the incidence of fatty liver in the present study. On similar lines a published study from China reported that oil (more than 44 grams per person per day) was significantly associated with increased risk of NAFLD (OR: 2.31; 95% CI: 1.26– 4.24) [22].
Oily foods have a high caloric content and generate excess of free fatty acids, triglycerides etc. which disturbs the metabolism of fatty acids along with hepatic accumulation of lipids in the liver. Due to the enhanced fatty acid metabolism, the harmful byproducts like ceramides, diacylglycerols sensitise the liver to injury and damage of hepatic cells [22,24].
Intake of evening snacks was an important risk factor for NAFLD. Intake of snacks contributes to excess caloric intake. Similar to the findings of our study in a recent study conducted in Iran it was reported that there is positive association between energy-dense nutrient-poor snacks intake and risk of NAFLD [3]. In a previous study saturated fatty acid was associated with increased risk of NAFLD [25]. A previous Indian study also reported a higher intake of fried food by NAFLD patients [22]. Similar associations of fatty liver with an intake of snacks have been reported in other published studies [26,27].
In this study the frequency of savory snack consumption more than twice/week was associated with NAFLD. In a study conducted in India high incidence of snack food consumption across all population age groups, gender, socio-economic levels, and locations was reported [28]. In another study it was reported that snack (savory and sweet) consumption was high among adults from sexes in both urban and rural locations of north and south India which was associated with obesity [29]. According to a recent study, the food environment in Indian society has undergone significant changes. These changes include greater availability and accessibility of processed foods, a shift away from the traditional Indian diet towards Western food, and an emphasis on food as a status symbol, an increase in food advertising, inappropriate eating habits, poor nutrition knowledge and greater convenience in food options [30].
Intake of alcohol, despite the exclusion criteria, was observed to be a risk factor. This may be observed due to reporting bias or Indian population may need a revised lower cut-off for alcohol intake different from western population. A cohort study reported that moderate alcohol intake was significantly and independently associated with the worsening of fibrosis, implying that even a moderate level of alcohol intake may be harmful (OR:1.29(1.18-1.40)) [31]. A review study conducted recently indicated that any amount of alcohol consumption can have negative effects on liver outcomes in individuals with Non-Alcoholic Fatty Liver Disease (NAFLD), including those who drink within recommended limits [32].
Conclusion
The risk factors found to be associated with NAFLD included waist circumference (>80 cm in females and >90 cm in males), low physical activity, edible oil (>25 g for males and >20 g for females), evening snack intake and intake of savory snacks in the evening, alcohol intake (even less than the cutoff), total cholesterol (≥ 200 mg) and family history of diabetes. These findings could form the base for our future studies on screening, prevention, and management of NAFLD. Hence with the correct quality of diet (like a choice of low calorie, low fat, low sugar, high fibre foods), inclusion of physical activity, keeping cardio-metabolic risk factors like dyslipidemias in check, maintaining body composition in the normal range, the incidence of NAFLD can be reduced. The overall lifestyle risk factors should be addressed in totality.
Limitations
The limitation included the use of ultrasound, which is the conventional method, noninvasive, and of low cost for screening of NAFLD as against liver biopsy which is considered the gold standard method of screening for NAFLD. Quantity of savory snacks was not taken therefore it is difficult to quantify the percentage of calories coming from these snacks. Alcohol intake was self-reported which may lead to reporting bias.
References
- Guo X, Yin X, Liu Z, Wang J. Non-Alcoholic Fatty Liver Disease (NAFLD) pathogenesis and natural products for prevention and treatment. Int J Mol Sci. 2022; 23(24): 15489
[Crossref] [Google Scholar] [Indexed]
- Berna G, Romero-Gomez M. The role of nutrition in non-alcoholic fatty liver disease: Pathophysiology and management. Liver Int. 2020; 40(S1): 102-108.
[Crossref] [Google Scholar] [Indexed]
- Yari Z, Cheraghpour M, Aghamohammadi V, Alipour M, Ghanei N, Hekmatdoost A. Energy-dense nutrient-poor snacks and risk of non-alcoholic fattyliver disease: a case–control study in Iran. BMC Res Notes. 2020; 13(1): 221.
[Crossref] [Google Scholar] [Indexed]
- Jarvis H, Keefe HO, Craig D, Stow D, Hanratty B, Anstee QM. Does moderate alcohol consumption accelerate the progression of liver disease in NAFLD? A systematic review and narrative synthesis. BMJ Open. 2022; 12(1): e049767.
[Crossref] [Google Scholar] [Indexed]
- Rastogi A, Prasad M, Ramalingam A, Kapil U. Non-alcoholic fatty liver disease and other non-communicable diseases: Time for an integrated approach. Indian J Community Heal. 2022;34(1): 1-8.
- Banerjee B. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS). 2017
- Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the american association for the study of liver diseases. Hepatology. 2018; 67(1): 328-357.
- Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the american association for the study of liver diseases, american college of gastroenterology, and the american gastroenterological association. Hepatology. 2012; 55(6): 2005-2023.
[Crossref] [Google Scholar] [Indexed]
- de Onis M, Habicht JP. Anthropometric reference data for international use: recommendations from a world health organization expert committee. Am J Clin Nutr. 1996; 64(4): 650-658.
[Crossref] [Google Scholar] [Indexed]
- Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009; 57(2): 163-170.
- Shalimar, Kumar R, Rout G, et al. Body mass index–based controlled attenuation parameter cut-offs for assessment of hepatic steatosis in non-alcoholic fatty liver disease. Indian J Gastroenterol. 2020; 39(1): 32-41.
[Crossref] [Google Scholar] [Indexed]
- World Health Organization. Global Physical Activity Questionnaire (GPAQ) Analysis Guide. 2012.
- Kp S, Srikantiah C. Sample Size estimation and Power analysis for Clinical research studies. J Hum Reprod Sci. 2012; 5: 7-13.
[Crossref] [Google Scholar] [Indexed]
- Saleem S. Modified Kuppuswamy socioeconomic scale updated for the year 2020. 2020; 7(1): 1-3
- Pan JJ, Fallon M. Gender and racial differences in nonalcoholic fatty liver disease. World J Hepatol. 2014; 6(5): 274-283.
[Crossref] [Google Scholar] [Indexed]
- Burra P, Bizzaro D, Gonta A, Shalaby S, Gambato M, Morelli MC, et al. Clinical impact of sexual dimorphism in non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH). Liver Int. 2021; 41(8): 1713-1733.
[Crossref] [Google Scholar] [Indexed]
- Bhatt DS, Misra A, Nigam P. Nutrition and physical activity in Asian Indians with non-alcoholic fatty liver: A case control study. Diabetes Metab Syndr Clin Res Rev. 2019; 13(2): 1271-1274.
[Crossref] [Google Scholar] [Indexed]
- Duseja A, Singh SP, Saraswat VA, et al. Non-alcoholic Fatty Liver Disease and metabolic syndrome-position paper of the indian national association for the study of the liver, endocrine society of India, Indian college of cardiology and Indian society of gastroenterology. J Clin Exp Hepatol. 2015; 5(1): 51-68.
[Crossref] [Google Scholar] [Indexed]
- Duseja A, Najmy S, Sachdev S, Pal A, Sharma RR, Marwah N, et al. High prevalence of non-alcoholic fatty liver disease among healthy male blood donors of urban India. JGH Open. 2019; 3(2): 133-139.
[Crossref] [Google Scholar] [Indexed]
- Singh SP, Singh A, Misra D, Misra B, Pati GK, Panigrahi MK, et al. Risk factors associated with non-alcoholic fatty liver disease in Indians: A case control study. J Clin Exp Hepatol. 2015; 5.
[Crossref] [Google Scholar] [Indexed]
- Swapna C, Madhusudan KS, Neena B, Naval KV, Pandey R Madhusudan K. Low and moderate level of physical activity is a risk. Indian J Appl Res. 2018; 3(1): 12-14.
- Majumdar A, Misra P, Sharma S, Kant S, Krishnan A, Pandav C. Prevalence of nonalcoholic fatty liver disease in an adult population in a rural community of Haryana, India. Indian J Public Health. 2016; 60(1): 26-33.
[Crossref] [Google Scholar] [Indexed]
- Jia F, Hu X, Kimura T, Tanaka N. Impact of dietary fat on the progression of liver fibrosis: lessons from animal and cell studies. Int J Mol Sci. 2021; 22(19): 10303.
[Crossref] [Google Scholar] [Indexed]
- Neuschwander-Tetri BA, Clark JM, Bass NM, et al. Clinical, laboratory and histological associations in adults with nonalcoholic fatty liver disease. Hepatology. 2010; 52(3): 913-924.
[Crossref] [Google Scholar] [Indexed]
- Chaturvedi S, Tripathi D, Vikram NK, Madhusudan KS, Pandey RM, Bhatia N. Association of nutrient intake with non-alcoholic fatty liver disease and liver steatosis in adult Indian population – A case control study. Hum Nutr Metab. 2023; 32: 200188.
- Adriano LS, Sampaio HA de C, Arruda SPM, Portela CLM, Melo MLP, Carioca AAF, et al. Healthy dietary pattern is inversely associated with non-alcoholic fatty liver disease in elderly. Br J Nutr. 2016; 115(12): 2189-2195.
- Rietman A, Sluik D, Feskens EJM, Kok FJ, Mensink M. Associations between dietary factors and markers of NAFLD in a general Dutch adult population. Eur J Clin Nutr. 2017; 72: 117-123.
[Crossref] [Google Scholar] [Indexed]
- Roy D, Boss R, Saroj S, Karandikar B, Pradhan M, Pandey H. Snack food consumption across the pune transect in india: a comparison of dietary behaviors based on consumer characteristics and locations. Nutrients. 2021; 13(12): 4325.
[Crossref] [Google Scholar] [Indexed]
- Ganpule A, Dubey M, Pandey H, et al. Snacking behavior and association with metabolic risk factors in adults from north and south India. J Nutr. 2023; 153(2): 523-531.
[Crossref] [Google Scholar] [Indexed]
- Kumar GS, Kulkarni M, Rathi N. evolving food choices among the urban indian middle-class: A qualitative study. Front Nutr. 2022; 9: 844413.
[Crossref] [Google Scholar] [Indexed]
- Chang Y, Cho YK, Kim Y, Sung E, Ahn J, Jung HS, et al. Nonheavy drinking and worsening of noninvasive fibrosis markers in nonalcoholic fatty liver disease: A cohort Study. Hepatology. 2019; 69(1): 64-75.
[Crossref] [Google Scholar] [Indexed]
- Cainelli F, Thao T, Pung C, Vento S. Alcohol? not for non-alcoholic fatty liver disease patients. Front med. 2020; 7: 14.
[Crossref] [Google Scholar] [Indexed]
Author Info
Swapna CHATURVEDI1, Divya TRIPATHI2, Naval Kishore VIKRAM2, Kumble S MADHUSUDHAN3, Ravindra Mohan PANDEY4 and Neena BHATIA5*2Department of Medicine, All India Institute of Medical Sciences, New Delhi, India
3Department of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi, India
4Department of Biostatistics, All India Institute of Medical Sciences, New Delhi, India
5Department of Food and Nutrition, University of Delhi, New Delhi, India
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
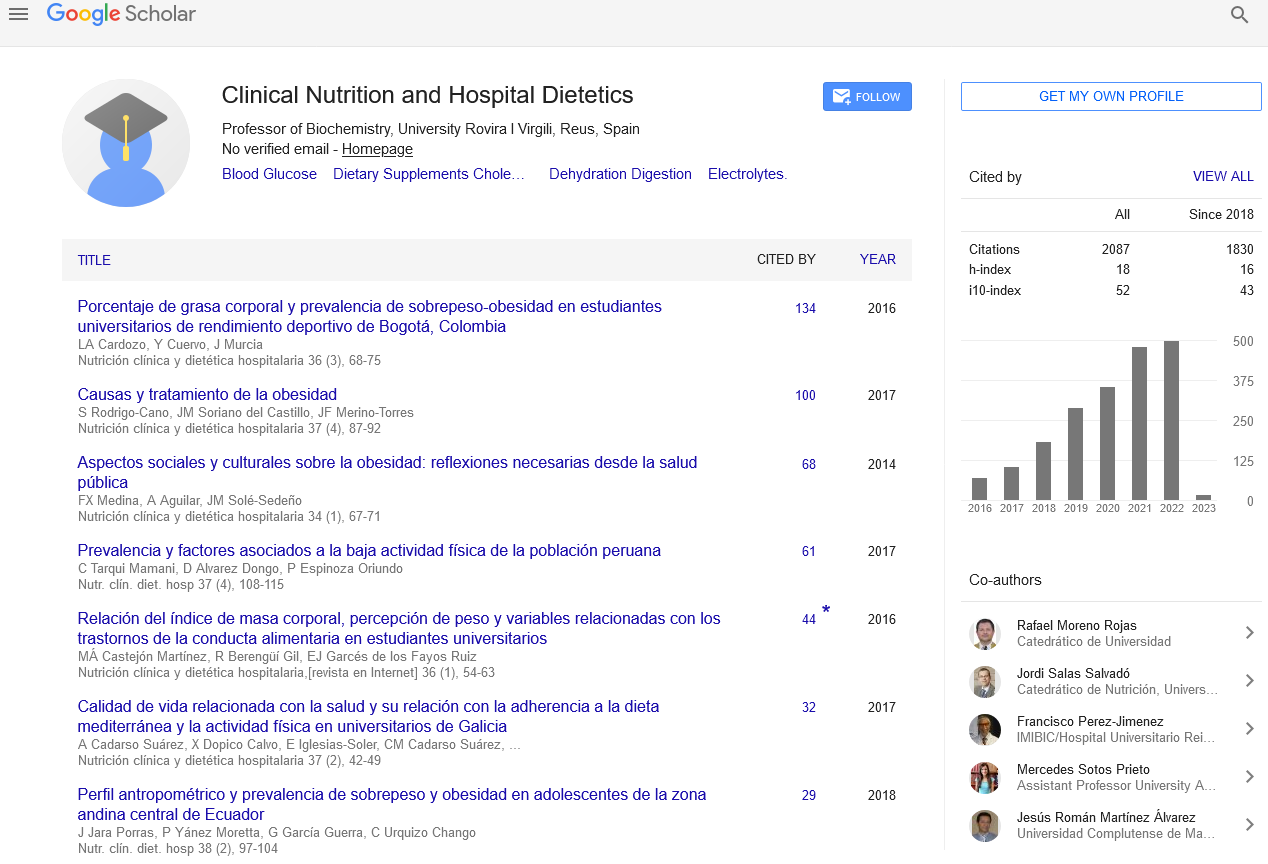
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics