Nutritional therapy in post laparatomy eksploration and omental flap due to gastric perforation with nasoduodenal tube: A case report
Research Article - (2023) Volume 43, Issue 2
Received: 10-Jul-2023, Manuscript No. CNHD-23-105353; Editor assigned: 12-Jul-2023, Pre QC No. CNHD-23-105353 (PQ); Reviewed: 26-Jul-2023, QC No. CNHD-23-105353; Revised: 02-Aug-2023, Manuscript No. CNHD-23-105353 (R); Published: 09-Aug-2023, DOI: 10.12873/0211-6057.43.02.199
Abstract
Gastric perforation is a full thickness injury to the gastic wall. All forms of perforation in the gastrointestinal are surgical emergency cases. Perforation complications that occur in patients with gastric ulcers. The objective of this case study is to explain the support of nutritional therapy in patients with post laparotomy eksploration and omental flap due to gastic perforation with nasoduodenal tube. Case report; A 71 year old male patient with moderate malnutrition was admitted to an Ear Nose Throat ward. Physical examination reveals loss of subcutaneous fat, muscle wasting, nasogastic tube for the decompression and nasoduodenal tube for nutrient intake, there was postoperative wound on stomach. Blood test shows anemia (8,3 g/dl), Leukocytosis (11.5 103/ul), hypoalbuminemia (2,4 g/dl), and moderate depletion immune system (1.173 103/ul). Nutrition therapy was given with a total calorie of 1800 kcal via nasoduodenal tube, protein 1.5-1,7 g/IBW/day, using low fiber blenderized food, a special oral nutrition supplements (hydrolized formula). An addtional supplementation in the form of zinc, multivitamins, curcuma, and snakehead fish extract capsules. After 12 days of nutritional treatment, the patient was discharged with adequate oral nutrition. Postoperative wound healed. Improved blood test results such as hemoglobin (8,3 to 11,4 g/dl), leukocytes (11.5 to 8.8 103/ ul), the immune status (1.173 to 1.628 103/ul), albumin (2,4 to 3,2 g/dl). In conclusion, a special nutritional therapy improved nutritional status and clinical outcome in post laparotomy eksploration with omental flap due to gastric perforation patients.
Keywords
Gastic perforation, Nutritional therapy, Nasoduodenal tube
Introduction
Gastric perforation is a full thickness injury to the organ wall. Gastric perforation can progress to chemical peritonitis caused by gastric acid leaking into the abdominal cavity. All forms of gastrointestinal perforation are surgical emergencies [1]. The most common etiology of gastric perforation is gastric ulcer and 10%-15% of patients with gastric ulcer may develop perforation. In perforated gastric ulcers, 6%-14% of cases are due to malignancy, in contrast to duodenal ulcers where the incidence of malignancy is found in almost zero cases. Nearly one million people worldwide are diagnosed with peptic ulcers every year. Complications occur in 10%-20% of patients, while 2%-14% of patients will develop perforation [2]. More than half cases are female, Perforations are most commonly found in the pre-pylorus (40%), duodenum (28%), and antrum (5%) [3-5]. Perforations Gastric cancer caused by gastric carcinoma is rare with an incidence of about 5% with the majority of patients being at an advanced stage (64%-88%). Perforation due to gastric malignancy is generally found in the greater curvature (77%) [2].
The two most common types of peptic ulcers are called “gastric ulcers” and “duodenal ulcers.” Many people with ulcers have no symptoms at all. Some ulcer patient experience abdominal pain. This pain often occurs in the upper abdomen. Sometimes food makes the pain better, and sometimes it makes it worse. Other symptoms include nausea, vomiting, or a feeling of bloating or fullness. The most important symptom caused by ulcers is related to bleeding. Bleeding from an ulcer can be slow and unnoticed or it can lead to life-threatening bleeding. An ulcer that bleeds slowly may not produce symptoms until the person becomes anaemic. Symptoms of anemia include fatigue, shortness of breath when exercising, and pale skin tone [6]. The two main causes of ulcers are Helicobacter pylori infection and a group of drugs known as Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). In Indonesia, peptic ulcers are the 10th leading cause of death in men aged 45-54 years, according to the BPPK Health Service in 2008 [7].
NSAIDs cause ulcers by interfering with the natural ability of the stomach and duodenum to protect themselves from stomach acid. NSAIDs can also interfere with blood clotting, which is especially important when the ulcer is bleeding. People who take NSAIDs for a long time and/ or in high doses, have a higher risk of developing ulcers. Every year Peptic Ulcer Disease (PUD) affects 4 million people worldwide. Complications are encountered in 10%-20% of these patients and 2%-14% of ulcers will perforate [8,9]. Perforated Peptic Ulcer (PPU) is quite rare, but life-threatening disease and mortality varies from 10%-40% [1,2]. Therefore, it is important to know the nutritional management of postoperative laparotomy patients due to gastric perforation in order to produce a good clinical outcome. In the following, we will discuss a postoperative exploratory laparotomy due to gastric perforation in a 71 year old man with anemia, leukocytosis, hypoalbuminemia, and immune system depletion.
Case Presentation
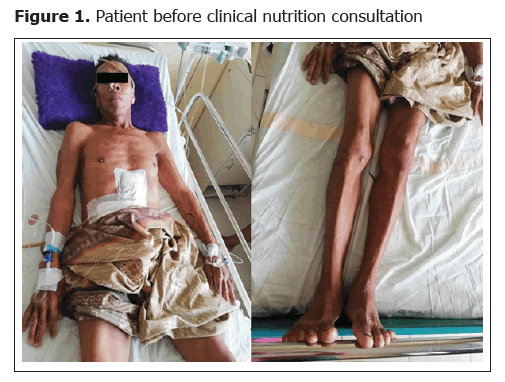
A 71 year old man was referred from Sinjai Hospital with a diagnosis of peritonitis et causa gastric perforation. The patient was not allowed to eat and drink orally since 2 days ago after an exploratory laparotomy was performed 3 days ago, the current intake is given via a nasoduodenal tube. History of food and drink intake via oral decreased since 1 month ago due to abdominal pain, nausea and vomiting. There has been abdominal pain since 1 month ago that comes and goes and has been getting worse since 7 days ago, continuously. There is a history of heartburn since the last 5 years that feels like it is being stabbed. History of painful swallowing, cough, shortness of breath, fever, and convulsions was denied. There has been weight loss since the last 1 month but not measurable. The patient has not had a bowel movement since 7 days ago and is urinating ± 1500 cc/24 hours through a clear yellow catheter. The patient has a history of gouty arthritis since 20 years ago, regularly taking over-the-counter pain relievers (Figure 1).
On physical examination the general condition of the patient appeared to be moderately ill, consciousness compos mentis, GCS 15 (E4M6V5). Vital signs showed blood pressure 110/80 mmHg, pulse 74x/minute, respiratory rate 18x/minute, and temperature 36.7°C. General physical examination found anemic conjunctiva (+/+), nasoduodenal and nasogastric tubes (for decompression), wasting in the lower extremities, other findings were within normal limits. Laboratory examination showed anemia (Hb 9 g/dl); leukocytes 16,900, TLC 774.4 × 103 and hypoalbuminemia (2.5 g/dl). Plain abdominal radiographs in 3 positions showed pneumoperitoneum ec gastric perforation signs of peritonitis and chest radiographs showed severe elevation of the diaphragm and cardiorespiratory image within normal limits. From the examination above, the nutritional diagnosis of the patient was moderate protein energy malnutrition (SGA score B), with leukocytosis, hypochromic microcytic anemia, severe immune system depletion, and hypoalbuminemia.
The nutritional intervention given was a diet of 1800 kcal with a macronutrient composition of 21% protein as much as 1.5 g/kgBW/day (94.5 g), 50% carbohydrates (225 grams), and 29% fat (58 grams). Nutrition therapy was given 30% KET (540 kcal) via enteral (dextrose 5% 5 x 20 cc) and parenterally in the form of Combiflex peri 1000 ml/24 hours and dextrose 5% 500 ml/24 hours intravenously. Give fluids as much as 1800 ml/24 hours.
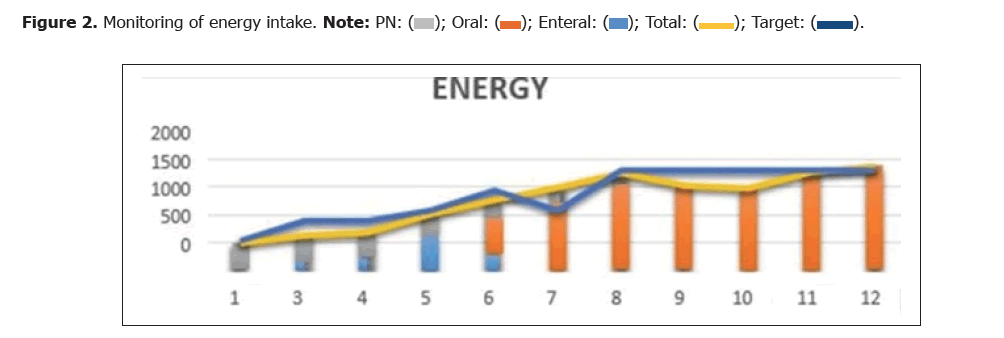
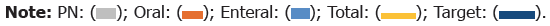
Correction of hypoalbuminemia with protein intake of 1.5 g/kg/day. Administered enteral zinc 20 mg/24 hours and neurobion 1 ampoule drip in 5% dextrose 500 ml/24 hours (Figure 2 and Figure 3) (Table 1 and Table 2).
| 1 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| PN | 480 | 480 | 480 | 420 | 336 | 294 | 170 | 0 | 0 | 0 | 0 |
| Oral | 0 | 0 | 0 | 0 | 667.37 | 1203 | 1541.2 | 1528 | 1480.25 | 1760.2 | 1870.4 |
| Enteral | 17 | 150 | 210 | 594.7 | 269.5 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 497 | 630 | 690 | 1014.35 | 1272.87 | 1497 | 1751.12 | 1528 | 1480.25 | 1764.2 | 1870.4 |
| Target | 540 | 900 | 900 | 1080 | 1440 | 1080 | 1800 | 1800 | 1800 | 1800 | 1800 |
| 1 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| PN | 40 | 40 | 40 | 30 | 24 | 21 | 15 | 50 | 0 | 0 | 0 |
| Oral | 0 | 0 | 0 | 0 | 37.6 | 54.8 | 71.3 | 41.6 | 80.3 | 89.4 | 91.6 |
| Enteral | 0 | 8.4 | 9.2 | 22.2 | 17.2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 40 | 48.4 | 49.2 | 52.2 | 64 | 75.8 | 86.3 | 91.6 | 80.3 | 89.4 | 91.6 |
| Target | 28.35 | 47.25 | 47.25 | 56.7 | 75.6 | 75.6 | 94.5 | 94.5 | 94.5 | 94.5 | 94.5 |
Results and Discussion
Malnutrition is a predictor of poor outcome after surgery and is associated with increased morbidity, mortality, Length of Stay (LOS), and hospital costs. Patients following certain major surgical procedures are at high risk of malnutrition due to metabolic stress. These patients need to have a nutritional care plan that begins with weight measurement or anthropometric measurements [10,11]. This patient was diagnosed as moderately malnourished based on the Subjective Global Assessment (SGA) criteria. SGA is divided into 3 categories, there are A (nutritious), B (mildly malnourished or suspected of being malnourished), and C (very malnourished). Some of the assessment points assessed in the SGA are body weight, food intake, gastrointestinal symptoms, functional capacity, subcutaneous fat, muscle atrophy, edema and ascites. The patient belongs to group B [4].
Anemia is a condition in which the Hemoglobin (Hb) is less than 14 g/dL in men or 12 g/dL in women. According to the WHO scoring system, it is classified as mild anemia (Hb 10 g/dl to normal), moderate (Hb 8-9.9 g/dl), severe (Hb 6.5-7.9 g/dl) and life-threatening (Hb<6.5 g/ dl) [8]. The patient has hypochromic microcytic anemia which can also be called iron deficiency anemia, which is characterized by decreased Hb levels, decreased levels of MCV and MCH. And from the anamnesis it was found that this patient had been taking NSAIDs for a long time which caused peptic ulcers that complicated to gastric perforation which caused bleeding (blood loss). Iron deficiency anemia can be caused by chronic bleeding. Chronic bleeding can come from the gastrointestinal tract (peptic ulcers, NSAID use, gastrointestinal cancer, diverticulosis, hemorrhoids, and hookworm infections), reproductive (menorrhagia or metorhagia), urinary tract (hematuria), or respiratory tract (hemoptysis). Other factors are nutritional factors, increased iron requirements, and impaired absorption due to gastrectomy, tropical sprue or chronic colitis.
In this case it was found that the Hb value of this patient before undergoing exploratory laparotomy and Omental Flap surgery was 6.3 g/dl and had received 4 bag PRC transfusions at the time of surgery and after surgery. So that, this patient had Hb result of 9.0 g/dl, with adequate intake and supplementation which then increased to 9.3 g/dl, then 10.6 g/dl and 11.4 g/dl when the patient went home. The nutritional intervention carried out in this patient to treat anemia was to provide adequate intake of macronutrients and micronutrients. Lack of energy and protein can lower the immune system so that the patient susceptible to infection which will increase pro-inflammatory cytokines then causes anemia. Adequate energy and protein intake is needed to reduce inflammation and increase iron absorption. The patient’s leukocyte at the time of consultation was 16,900 L, when the patient went home the lukocyte were 8800 L. The acute phase response which including fever, can increase the leukocyte count even in the absence of infection, increase the amount of acute phase protein (Creactive protein and others) and decrease serum albumin levels. This is due to the presence of cytokines. Leukocytosis in this patient was treated with antibiotics by digestive surgery colleague and nutritional therapy given was zinc 20 mg every 24 hours, vitamin B complex 2 tabs every 8 hours, vitamin C 50 mg every 8 hours, curcuma 400 mg every 8 hours [12].
This patient was diagnosed with severe hypoalbuminemia at the time of consultation with a level of 2.4 g/dl, and was given Human Albumin 25% 100 ml every 24 hours intravenously. However, the results obtained post-correction are still 2.4 g/dl. So that the protein composition was given at 1.5 g/KgBBI/day obtained from the initial intake, such as parenteral nutrition with combiflex peri 1000 ml/24 hours intrevenously. Then, patient were then given with enteral intake (nasoduodenal tube) in the form of full liquid peptisol, because the patient complained of bloating after being given ONS peptisol, enteral intake was replaced with ONS Peptamen which is an oligomeric nutrition. The next intake is given with filtered food until the NGT is released, then protein intake is given orally and parenterally according to the patient’s gastrointestinal tolerance. Patients were also given snakehead fish extract capsules, 2 capsules every 8 hours. Zinc is given as an anti-oxidant that will protect cells, accelerate wound healing, regulate expression in lymphocytes and proteins and improve appetite [13]. Albumin is a negative acute phase protein synthesized by the liver which is influenced by nutritional intake, especially protein deficiency and acute inflammation [14]. Hypoalbuminemia associated with inflammation because inflammation increases capillary permeability and release of serum albumin, leading to expansion of the interstitial space and an increase in the volume of distribution of albumin. Hypoalbuminemia, is the result of a reflective state of inflammation, which interferes with adequate response to events such as surgery or chemotherapy, and is associated with poor quality of life and reduced longevity [15,16]. In injury, nearly every type of immune cell appears, producing cytokines and growth factors that support the healing process [17,18].
At the time of consultation, the patient found a severe depletion of the immune system where the value of Total Lymphocyte Count (TLC) was 777.4 which indicate a severe depletion of the immune system. After a few days of treatment, there was an improvement from this depletion of the immune system which improved from severe to mild depletion of the immune system which then at the end of treatment the value of a normal TLC was 1628. A decrease in the body’s immune system is one of the body’s mechanisms to reduce inflammation rate. TLC level is an indicator of immune function that can be used as a screening and assessment of nutritional status. The high level of inflammation caused by the production of pro-inflammatory cytokines can exert an immunosuppressive effect. Patients with malnutrition will reduce immune function [19]. Completing total energy needs is a therapy to increase the body’s immune system. Zinc supplementation can increase the body’s immune system by activating B cells and T cells.20 The nutritional therapy given is zinc supplementation 20 mg every 24 hours, vitamin A 6000 IU every 24 hours, vitamin C 50 mg every 8 hours, and curcuma 400 mg every 8 hours. Zinc has also been reported for its ability to increase the activity of the enzyme Superoxide Dismutase (SOD) and is able to increase all types of T cells, allowing T cells to proliferate and differentiate which ultimately stimulates cellular enzyme activity. Vitamin A plays a role in stimulating epithelialization and the immune system, on monocyte and macrophage aggregation, increasing the number of macrophages and monocytes in wounds, supporting mucosal and epithelial surfaces, increasing collagen formation, protecting against the adverse effects of glucocorticoids at a dose of 10,000-15,000 IU.21
Conclusion
A 71-year-old man was consulted by the digestive surgery department with a diagnosis of post-exploratory laparotomy on day 2 with omental flap et causa gastric perforation, not allowed to eat and drink orally since 2 days ago after surgery exploratory laparotomy + omental flap, the current intake is given via nasoduodenal tube. In this patient, the energy requirement was corrected with energy of 1800 kcal/day, with the administration gradually until it reached the target. Nutritional therapy is given to improve the nutritional status and metabolic status of the patient by providing nutrition with 1800 kcal of energy with a composition of 50% carbohydrates (225 grams), 21% protein (94.5 grams), and 29% fat (554.8 grams). Initial management of the patient was done by providing enteral nutrition via nasoduodenal tube because the patient could not eat or drink orally and the stomach was temporarily decompressed and slowly increased until the KET was achieved. Malnutrition in patients with gastric perforation can affect response to therapy, quality of life and quality of life mortality optimal nutrition intervention according to patient needs, monitoring and education can accelerate the healing process, length of stay and improve the quality of life of patients. Good health team collaboration including doctors, nurses, nutritionists and family support is very important in comprehensive and integrated patient management, so as to accelerate clinical and metabolic improvement of patients.
References
- American College of Gastroenterology. Peptic Ulcer Disease. 2022.
- Baker SP, O'neill B. The injury severity score: an update. J Trauma. 1976; 16(11):882-885.
[Crossref] [Google Scholar] [Indexed]
- Baron JH. Peptic ulcer. Mt Sinai J Med. 2000; 67(1):58-62.
[Indexed]
- Bertleff MJOE, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg. 2010; 27(3):161-169.
[Crossref] [Google Scholar] [Indexed]
- Rainsford KD. Ibuprofen: A Critical Bibliographic Review. CRC Press. 2003; 571.
- Brune K, Glatt M, Graf P. Mechanisms of action of anti-inflammatory drugs. Gen Pharmacol. 1976; 7(1):27-33.
[Crossref] [Google Scholar] [Indexed]
- Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition - An ESPEN Consensus Statement. Clin Nutr. 2015; 34(3):335-40.
[Crossref] [Google Scholar] [Indexed]
- Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC. Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion. 2011; 84(2):102-13.
[Crossref] [Google Scholar] [Indexed]
- Leeman MF, Skouras C, Paterson-Brown S. The management of perforated gastric ulcers. Int J Surg Lond Engl. 2013; 11(4):322-324.
[Crossref] [Google Scholar] [Indexed]
- Lim RHG, Tay CM, Wong B, Chong CS, Kono K, So JBY, et al. Perforated early gastric cancer: uncommon and easily missed a case report and review of literature. J Gastric Cancer. Maret 2013; 13(1):65-68.
[Crossref] [Google Scholar] [Indexed]
- Muscaritoli M, Anker SD, Argilés J, Aversa Z, Bauer JM, Biolo G, et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics.” Clin Nutr Edinb Scotl. 2010; 29(2):154-159.
[Crossref] [Google Scholar] [Indexed]
- Gabbe BJ, Cameron PA, Wolfe R. TRISS: does it get better than this? Acad Emerg Med. 2004; 11(2):181-186.
[Crossref] [Google Scholar] [Indexed]
- Kasim VN, Pateda SM, Hadju V, Jafar N. Supplementation of snakehead fish albumin extract on nutritional status and immunity of stroke patients. J Gizi Klin Indones. 2017; 13(3):91-98.
- Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 2017; 36(1): 49-64.
[Crossref] [Google Scholar] [Indexed]
- Riddell MR, Winkler-Lowen B, Chakrabarti S, Dunk C, Davidge ST, Guilbert LJ. The characterization of fibrocyte-like cells: a novel fibroblastic cell of the placenta. Placenta. 2012; 33(3):143–50.
[Crossref] [Google Scholar] [Indexed]
- Selkov SA, Selutin AV, Pavlova OM, Khromov-Borisov NN, Pavlov OV. Comparative phenotypic characterization of human cord blood monocytes and placental macrophages at term. Placenta. 2013; 34(9):836-839.
[Crossref] [Google Scholar] [Indexed]
- Grimble RF. Basics in clinical nutrition: Immunonutrition-Nutrients which influence immunity: Effect and mechanism of action. Eur E-J Clin Nutr Metab. 1 Februari 2009; 4(1):10-13.
- Gibson RS. Principles of Nutritional Assessment. Oxford University Press. 2005; 930
- Saghaleini SH, Dehghan K, Shadvar K, Sanaie S, Mahmoodpoor A, Ostadi Z. Pressure Ulcer and Nutrition. Indian J Crit Care Med. 2018; 22(4):283-239.
[Crossref] [Google Scholar] [Indexed]
Author Info
Urfa PATUNDRU1*, Suryani AS’AD1,2, Mardiana MADJID1,4 and Asrini SAFITRI32Department of Nutrition, Muhammadiyah University School of Medicine, Makassar, Indonesia
3Department of Nutrition, Indonesian Muslim University School of Medicine, Makassar, Indonesia
4Department of Nutrition, Wahidin Sudirohusodo Hospital, Makassar, Indonesia
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics