The importance of precision nutrition in binge eating disorder
Review Article - (2024) Volume 0, Issue 0
Received: 10-Sep-2024, Manuscript No. CNHD-24-147699; Editor assigned: 13-Sep-2024, Pre QC No. CNHD-24-147699 (PQ); Reviewed: 30-Sep-2024, QC No. CNHD-24-147699; Revised: 07-Oct-2024, Manuscript No. CNHD-24-147699 (R); Published: 14-Oct-2024, DOI: 10.12873/0211-6057.44. S1.007
Abstract
Binge eating disorder is considered the most prevalent disorder in the athletic population (compared to anorexia and bulimia nervosa), however, there is still a lot of research to be done, especially from an interdisciplinary perspective. For this reason, in this article we present the most updated research on genetic predisposition, eating behavior, relationship with stress and other eating diseases or addiction to sport and analyze whether precision nutrition offers tools to offer effective work guidelines from its scope. In the literature consulted, factors in which nutrition can work in both prevention and treatment are observed. For this reason, knowing the genetic factors, function of the microbiota and psychosocial aspects of each athlete could be important to prevent the appearance of eating disorder in general and binge eating disorder. However, although precision nutrition may be key, interdisciplinary work is also essential (psychiatry, psychology, nursing, nutrition and other specialists depending on the need). And, although future research will provide more information in this regard, it is known that the Mediterranean Diet pattern still offers an important preventive tool
Keywords
BED (Binge Eating Disorder), ED (Eating Disorder), Athletes, Precision Nutrition, Prevention
Introduction
The main Eating Disorders (ED) described by the Diagnostic and Statistical manual of Mental disorders (DSM) are Anorexia Nervosa (AN), Bulimia Nervosa (BN) and Binge Eating Disorder (BED) [1]. Binge Eating Disorder (BED) is the most common among Western society, with a prevalence between 2% and 4%, and may be underdiagnosed because it is confused with overweight or obesity [2,3]. Broadly speaking, it is characterized by recurrent binge eating (≥ 1 time per week, minimum for 3 months), brief (≤ 2 h) and distressing, during which patients feel a lack of control in which they consume large amounts of food compared to most people in similar circumstances [1].
In the athletic setting, BED prevalence rates are believed to be higher than among society in general due to strict requirements regarding weight and body composition, prolonged caloric restriction, stressors linked to competitions, and even social and media pressures [4]. Moreover, it seems to be a disorder of similar prevalence among men and women (unlike the mostly female AN or BN) [3,5]. However, there is still much research to be done on this topic and it should be taken into account that specific circumstances of athletes can induce episodes of binge eating without being considered BED, such as a boxer’s eating after pre-competition weigh-in [6].
In the present article we analyze the main causes related to ED in athletes, especially BED, to discuss the role of precision nutrition in the emergence, prevalence and perhaps prevention of this disease.
Literature Review
BED and genetic predisposition
Genetics plays a fundamental role in the manifestation of BED. Specifically, genetic factors predispose approximately 41% to 57% to BED [7]. This makes research in this field necessary, however, there is still little literature compared to AN or BN and the one that exists does not yet show a clear focus due to the lack of information regarding the underlying physiological mechanisms [8-9]. In particular, certain dopaminergic and serotonergic SNPs have been studied for the relationship between nervous system influence and BED (Ankyrin repeat and kinase domain containing, Dopamine receptor D2, Opioid Receptor Mu1, Serotonin transporter gene) [10-15]. Also related to fat mass (fat mass and obesity associated gene, fatty acid binding protein), regulation of appetite and satiety (Taste Receptor Type 1 Member 2, Melanocortin 4 Receptor, Ghrelin and Obestatin Prepropeptide) or the circadian clock (Circadian Locomotor Output Cycles Kaput) influencing the matching of food intakes to physiological needs [16-23]. Nevertheless, and despite the different lines opened in the field of genetics, we think that these studies do not end up offering complete solutions for the existence of BEDs either. Other research shows that there is a relationship between microbial genetics, appetite and body weight, therefore, the Binge Eating Genetics Initiative (BEGIN) has emerged as an innovation in terms of BED, a multidimensional research that examines the interaction of the genome with the gut microbiota and phenotypic data to establish treatment responses to BED and BN [24,25].
Thus, we argue that the fields of nutrigenetics (variations in the gene that induce certain dietary behaviors) and nutrigenomics (effects that nutrients ingested through the food intake exert on the individual’s own genome) are of great importance [16,26,27]. However, due to the complexity of mechanisms and influential factors, we wonder if a diet based on these results can be really practical and/or effective.
BED and caloric restriction in an athletic population: The fact that BED in athletes is linked to caloric restriction may help prevent its appearance. However, this alone is not the determining factor. Nevertheless, we raise the possibility that those in charge of preparing the athlete’s diet should propose nutritional strategies based both on improving performance and avoiding an insufficient intake of nutrients that could lead to harmful situations for their health. There is sufficient scientific evidence to demonstrate that prolonged caloric restriction (as may occur in dance, gymnastics, boxing, athletics, etc.) alters hunger and satiety signals, generating a desire to overeat, for example, related to low levels of leptin and insulin [11,17]. In addition, a diet insufficient in certain macros and micronutrients (proteins, fats, carbohydrates, vitamins and minerals) can promote increased appetite [28,29].
There are also studies that highlight the modulation through food of the microbiota-intestine-brain axis, so that prolonged situations of food restriction produce dysbiosis related to ED [30-32]. However, we understand that the cause-effect direction is not yet clear due to the fact that, on the one hand, there are those who highlight that modifications in the bacterial composition of the intestine produce changes in eating behavior [33,34]. And, on the other hand, that situations of ED presence describe a microbial profile different that shown when the disease has been overcome [35]. However, most studies in this regard are performed in murine models and, in addition the composition of the intestinal ecosystem is unique to each individual, so working individually on each bacterial strain may be an error that could be mitigated by analyzing the functionality of digestive system as a whole [36].
BED and stress in the athletic population: In BED, periods of stress have been associated with those of binge eating, perhaps due to variations in terms of brain receptors, hormonal or even the aforementioned relationship in terms of the microbiota-intestine-brain axis [26,36,37].
Specifically, the athlete population is subjected to stress related to excessive exercise, caloric restriction, competition pressures, etc. [38]. Which may emphasize the predisposition to manifest this disorder. We advocate for an adequate psychological intervention not only linked to performance but also in the prevention of this type of disease, with emphasis on the promotion of joint work with the nutritionist and trainer, the latter being vital in the safety and confidence of the athlete [39]. Clear examples can be seen in cases published in press in which the athletes describe the pressure from their coach to have a lower weight. In addition, this extends to society (and the media), which establish standards about the ideal physique of athletes, and they are not even aware of the pressure exerted [4].
BED and sports addiction: Addiction disorders are more prevalent in patients with ED than in the general population and vice versa so it is assumed that there is a common intrinsic component linked to addiction [13]. We argue that, in the case of the athlete population, this addictive behavior can materialize in excessive sports practices, as for example shown in the study by Monserrat-Hernández et al., regarding long-distance runners (more hours, more training sessions and inadequate recovery rest) [40]. At this point it should be noted that the obsession with physical exercise can lead to and/or strengthen an ED or vice versa, so there is controversy as to whether the most susceptible groups to take part in a sport that requires a certain physique are people with ED (more research has been done on AN) [41]. It is argued that excessive exercise and ED represent expressions of the same preoccupation with body control, and that excessive exercise may be perceived as a more acceptable alternative to an eating disorder, but how can this be measured in a sport where excessive exercise is a daily routine?
In view of this, we believe that it would be advisable for coaches and sports psychologists to deal with and respond in advance to the presence of warning signs or to carry out assessments regarding motivation towards sport.
Relation between BED, AN and BN in the athletic population
In general, ED share altered eating behavior and times of food restriction, so it may be normal that they acquire a spectral functionality, fluctuating among those who suffer from them (a person with AN can have BN and the same can happen with BED) [1,42]. Specifically, and due to the lack of sufficient research, we consider the need to increase research in this regard. Athletes, in times of high stress and caloric restriction can manifest episodes of binge eating using a high frequency of training as a purge. We also think that athletes who have been very strict nutritionally and subjected to stress during periods of competition, during rest periods or at the end of their career compensate this situation by eating, thus considering an edorexia [43]. For all these reasons, we consider it especially important to work on the prevention of ED as a whole.
Discussion
At this point, we consider that the need for interdisciplinary work in the prevention of any ED in sport is more than evident. Just as the team that surrounds the athlete is motivated by maximizing their performance, this team must be aware of prevention against the manifestation of disorders of this nature [39]. And, to this end, we consider it vitally important to establish work protocols in the areas of intervention (psychological, nutritional and training). The implementation of specific tests to detect addiction to sport, motivation towards it, as well as the danger of suffering from ED should be implemented constantly at the beginning of each season.
Similarly, the dimensions related to the possible manifestation of the disorder should be analyzed. In this regard, the undersigned team has validated a questionnaire to measure the risk of developing ED taking into account physical, psychological and social dimensions [44]. In this way, simpler and more focused lines could be established for effective intervention.
Specifically, nutritional planning should be considered more than a mere instrument, it has to be seen as an important factor in both prevention and improvement of the performance and health of athletes. For this reason, we put forward the need to carry out exhaustive controls regarding the adequate supply of nutrients throughout the season. At the level of macronutrients, it must be adapted to the needs of each athlete in the specific period, both carbohydrates and fats and proteins play a fundamental role [5,45]. In the case of micronutrients, there is sufficient scientific evidence that an adequate intake of vitamins D, E, C, B2, B3, B6 and B9 improves psychological well-being through their action as cofactors and coenzymes in the metabolic regulation of tryptophan or in brain methylation processes important in moodinfluencing brain functions [46,47].
In a generalized way and according to the literature analyzed, it could be suggested to reduce the total glycemic load of carbohydrates and their Glycemic Index (GI) except in the meal prior to training or competition. Excessive consumption of sweeteners and processed foods (even if they are considered healthy) should be avoided, giving priority to natural foods. A diet low in high GI carbohydrates, adequate levels of protein, low in saturated fats and high in monounsaturated fats reduces inflammatory processes and lipid profile without the need to establish excessively restrictive diets [48]. In this regard, we believe that providing sufficient knowledge to athletes about the foods they should eat can promote less strict diets, as well as establishing menus appropriate to dietary preferences. This can be a great challenge for the field of nutrition education.
Guidelines and recommendations for precisión nutrition in Binge Eating Disorder (BED)
Genes analyzed with possible predisposition to BED (Specific SNP):
• FTO (Fat Mass and obesity associated gene): Promotes the increase of fatty foods
• TAST1R2 (Taste Receptor Type 1 Member 2): Regulates the sense of taste
• GLUT2 (Glucose transporter 2): Under detection of blood glucose
• DRD2 (Dopamine Receptor D2) and DRD3 (Dopamine Receptor D3): Linked to dopamine, promotes over eating
• ANKK1 (Ankyrin repeat and kinase domain containing I): Relation with other addictions
• OPRM1 (Opioid Receptor Mu 1): Related to the opioid system. Eating for a sense of well being
• FABP2 (Fatty Acid Binding Protein 2): Related to hormonal regulation (leptin and insulin). Increased appetite
• CLOCK (Carcadian Locomotor Output Cycles Kaput 1): Hormonal imbalances related to circadian rhythms
• MCR4R ( Melanocortin 4 Receptor): Related to increased snacking and prevalence of binge Eating
• Other genes in research process: BDNF (Brain-derived Neurotrophic Factor), OXTR (Oxytocin Receptor), FAAH (Fatty Acid Amide Hydrolase), 5-HTTLPR (Serotonin-transporter Gene), SL6A4 (Solute carrier Family 6 member 4), GHRL (Ghrelin and Obestatin Prepropeptide)
Characteristics of microbiota:
• Increased production of SCFA (Propionate, butyrate, acetate)
• Maintaining adequate levels of lactobacillus and bifidobacterium
Micronutrients influencing stress and anxiety levels:
• Vitamin B6 and B12: For adequate functioning of the nervous system
• Vitamin C: Stimulate the adrenal glands (cortisol)
• Vitamin D: Ally in physiological stress processes
• Magnesium, calcium, potassium and zinc : Important for sympathetic and parasympathetic balance, rest and recovery in stress conditions
• Selenium and Vitamin E: To reduce oxidative stress in high-performance sport
• Tryptophan: Regulates the nervous system and favours rest and recuperation
• Glutamine: Contributor to the regeneration and protection of the intestinal wall
Effective amounts of macronutrients to avoid deficits in restrictive diets:
• Carbohydrates
• Recovery after 4 hours of moderate effort : 0.7 g/kg of weight, intervals of 2 h
• Optimal muscle glycogen recovery after exercise: 7 g-12 g/kg weight /day
• HC load prior to exercise of less than 90 min (36 h-48 h before) :10 g-12 g/kg bw/day
• Rapid recovery when the time between sessions is less than 8 h : 1 g-12 g/kg body weight immediately after and repeat ever hour until normality is established
• HC availability before prolonged training : 1 g-4 g/kg body weight 1-2 h before
• During sustained high-intensity exercise (45-75 min) : 30 g-60 g HC per hour
• During ultra-endurance exercise: 30 g-60 g of CH in the first hour, 60 g from the second hour and 90 g from the third hour
• During moderate intensity exercise or intervals of more than 1 h:0.5 g-1 g/kg body weight
• During high intensity exercise 1 g-1.5 g/kg body weight
• Fats : Increase consumption of monounsaturated fats, reduce consumption of saturated fats
• Omega 3 aids rest and recovery
• Optimal balance between omega 3 and omega 6
• Proteins
• Total daily intake of 1.2 g to 2.0 g protein per kilogram body weight (g/kg), appropriate to training intensity. Encourage elite athletes to adhere closer to the 2.0 g/kg side of this range, particularly during periods of higher volume training
• Variability in protein intake: fish, dairy, eggs, legumes, nuts, and meat
Psychosocial factors:
• Nutritional education to control stress generated by food
• Interdisciplinary work: Adapting nutritional guidelines to the advice of the sports psychologist
• Adapting the diet to the characteristics of each sports person. Including culinary tastes
• Avoid prolonged restrictions and food prohibition
Conclusion
With all that has been mentioned in this article, we can draw the following conclusions regarding nutritional intervention in BED: Nutrition is an important tool in the prevention of BED in athletes. The adequacy of macronutrients to the specificities of each athlete and training period is fundamental to correctly regulate the hunger-satiety processes. A correct intake of micronutrients will help to improve emotional well-being and prevent stress episodes linked to BED. Genetic analysis of predisposition to certain nutritional behaviors is having an increasing impact and is proving valid in diagnostic processes and personalized intervention.
Author Contributions
D.S.G: Writing–review and editing, Conceptualization, Methodology, Project administration; J.C.O: Writing– review and editing, Conceptualization, Methodology; M.M.H: Writing–original draft, Conceptualization, Methodology; review and editing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Branjerdporn G, Meredith P, Strong J, Garcia J, Brockington IF, Aucamp HM, et al. Diagnostic and statistical manual of mental disorders: DSM-5™, 5th ed. Americ Psychiat Assoc. 2013.
- Welch E, Jangmo A, Thornton LM, Norring C, von Hausswolff-Juhlin Y, Herman BK, et al. Treatment-seeking patients with binge-eating disorder in the Swedish national registers: Clinical course and psychiatric comorbidity. BMC Psych. 2016;16:1-8.
[Crossref] [Google Scholar] [Indexed]
- Marek RJ, Benâ?ÂÂPorath YS, Ashton K, Heinberg LJ. Impact of using DSMâ?ÂÂ5 criteria for diagnosing binge eating disorder in bariatric surgery candidates: Change in prevalence rate, demographic characteristics, and scores on the Minnesota Multiphasic Personality Inventory–2 Restructured Form (MMPIâ?ÂÂ2â?ÂÂRF). Int J Eat Disord. 2014;47(5):553-557.
[Crossref] [Google Scholar] [Indexed]
- Pascoe M, Pankowiak A, Woessner M, Brockett CL, Hanlon C, Spaaij R, et al. Gender-specific psychosocial stressors influencing mental health among women elite and semielite athletes: A narrative review. Br J Sports Med. 2022;56(23):1381-1387.
[Crossref] [Google Scholar] [Indexed]
- Trace SE, Thornton LM, Root TL, Mazzeo SE, Lichtenstein P, Pedersen NL, et al. Effects of reducing the frequency and duration criteria for binge eating on lifetime prevalence of bulimia nervosa and binge eating disorder: Implications for DSMâ?ÂÂ5. Int J Eat Disord. 2012;45(4):531-536.
[Crossref] [Google Scholar] [Indexed]
- Checa Olmos JC, Monserrat Hernández M, Belmonte García T, Jiménez Rodríguez D, Rodríguez Martínez A, Berenguel Martínez P, et al. Social and individual factors associated with eating disorders in young athletes: Effects on concentration and fatigue. Sports. 2023;11(7):122.
[Crossref] [Google Scholar] [Indexed]
- Yilmaz Z, Hardaway JA, Bulik CM. Genetics and epigenetics of eating disorders. Adv Genom Genet. 2015;5:131-150.
[Crossref] [Google Scholar] [Indexed]
- Watson HJ, Yilmaz Z, Thornton LM, Hübel C, Coleman JR, Gaspar HA, et al. Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa. Nat Genet. 2019;51(8):1207-1214.
[Crossref] [Google Scholar] [Indexed]
- Heidinger BA, Cameron JD, Vaillancourt R, De Lisio M, Ngu M, Tasca GA, et al. No association between dopaminergic polymorphisms and response to treatment of binge-eating disorder. Gene. 2021;781:145538.
[Crossref] [Google Scholar] [Indexed]
- González LM, Mota-Zamorano S, García-Herráiz A, López-Nevado E, Gervasini G. Genetic variants in dopamine pathways affect personality dimensions displayed by patients with eating disorders. Eat Weight Disord. 2021;26:93-101.
[Crossref] [Google Scholar] [Indexed]
- Koren R, Duncan AE, Munn-Chernoff MA, Bucholz KK, Lynskey MT, Heath AC, et al. Preliminary evidence for the role of HTR2A variants in binge eating in young women. Psychiat Genet. 2014;24(1):28-33.
[Crossref] [Google Scholar] [Indexed]
- Leehr EJ, Schag K, Brückmann C, Plewnia C, Zipfel S, Nieratschker V, et al. A putative association of COMT Val (108/158) met with impulsivity in binge eating disorder. Eur Eat Disord Rev. 2016;24(2):169-173.
[Crossref] [Google Scholar] [Indexed]
- Munnâ?ÂÂChernoff MA, Baker JH. A primer on the genetics of comorbid eating disorders and substance use disorders. Eur Eat Disord Rev. 2016;24(2):91-100.
[Crossref] [Google Scholar] [Indexed]
- Nonino CB, Barato M, Ferreira FC, Delfino HB, Noronha NY, Nicoletti CF, et al. DRD2 and BDNF polymorphisms are associated with binge eating disorder in patients with weight regain after bariatric surgery. Eat Weight Disord. 2022;27(4):1505-1512.
[Crossref] [Google Scholar] [Indexed]
- Palacios A, Canto P, Tejeda ME, Stephano S, Luján H, García-García E, et al. Complete sequence of the ANKK1 gene in Mexican-Mestizo individuals with obesity, with or without binge eating disorder. Eur Psychiatry. 2018;54:59-64.
[Crossref] [Google Scholar] [Indexed]
- Manfredi L, Accoto A, Couyoumdjian A, Conversi D. A systematic review of genetic polymorphisms associated with binge eating disorder. Nutrient. 2021;13(3):848.
[Crossref] [Google Scholar] [Indexed]
- Micali N, Field AE, Treasure JL, Evans DM. Are obesity risk genes associated with binge eating in adolescence?. Obesity. 2015;23(8):1729-1736.
[Crossref] [Google Scholar] [Indexed]
- Cameron JD, Tasca GA, Little J, Chyurlia L, Ritchie K, Yeh E, et al. Effects of fat mass and obesity-associated FTO gene polymorphisms on binge eating in women with binge-eating disorder: The moderating influence of attachment style. Nutrition. 2019;61:208-212.
[Crossref] [Google Scholar] [Indexed]
- Palmeira L, Cunha M, Padez C, Alvarez M, Pinto-Gouveia J, Manco L. Association study of variants in genes FTO, SLC6A4, DRD2, BDNF and GHRL with Binge Eating Disorder (BED) in Portuguese women. Psychiatry Res. 2019;273:309-311. [Crossref]
- Duarte AC, da Silva NR, Santos Gonçalves VS, Corgosinho FC, de Carvalho KM, Horst MA. The influence of single nucleotide polymorphisms on body weight trajectory after bariatric surgery: A systematic review. Curr Obesity Rep. 2023;12(3):280-307.
[Crossref] [Google Scholar] [Indexed]
- Kops NL, Vivan MA, Horvath JD, de Castro ML, Friedman R. FABP2, LEPR223, LEP656, and FTO polymorphisms: Effect on weight loss 2 years after bariatric surgery. Obesity Surgery. 2018;28:2705-2711.
[Crossref] [Google Scholar] [Indexed]
- Magno FC, Guaraná HC, da Fonseca AC, Pedrosa AP, Zembrzuski VM, Cabello PH, et al. Association of the MC4R rs17782313 polymorphism with plasma ghrelin, leptin, IL6 and TNFα concentrations, food intake and eating behaviors in morbidly obese women. Eat Weight Disord. 2021;26:1079-1087.
[Crossref] [Google Scholar] [Indexed]
- Monteleone P, Tortorella A, Docimo L, Maldonato MN, Canestrelli B, De Luca L, et al. Investigation of 3111T/C polymorphism of the CLOCK gene in obese individuals with or without binge eating disorder: Association with higher body mass index. Neurosci Lett. 2008;435(1):30-33.
[Crossref] [Google Scholar] [Indexed]
- Himmerich H, Minkwitz J, C Kirkby K. Weight gain and metabolic changes during treatment with antipsychotics and antidepressants. Endocr Metab Immune Disord Drug Targets. 2015;15(4):252-260.
[Crossref] [Google Scholar] [Indexed]
- Bulik CM, Butner JE, Tregarthen J, Thornton LM, Flatt RE, Smith T, et al. The Binge Eating Genetics Initiative (BEGIN): Study protocol. BMC Psychiatry. 2020;20:1-9.
[Crossref] [Google Scholar] [Indexed]
- Herman A, Bajaka A. The role of the intestinal microbiota in eating disorders–bulimia nervosa and binge eating disorder. Psychiatry Res. 2021;300:113923.
[Crossref] [Google Scholar] [Indexed]
- Rivera-Iñiguez I, Panduro A, Villaseñor-Bayardo SJ, Sepulveda-Villegas M, Ojeda-Granados C, Roman S. Influence of a nutrigenetic intervention on self-efficacy, emotions, and rewarding behaviors in unhealthy eating among Mexicans: An exploratory pilot study. Nutrients. 2022;14(1):213.
[Crossref] [Google Scholar] [Indexed]
- Pedram P, Wadden D, Amini P, Gulliver W, Randell E, Cahill F, et al. Food addiction: Its prevalence and significant association with obesity in the general population. Plos One. 2013;8(9):e74832.
[Crossref] [Google Scholar] [Indexed]
- Lugo NT. El zinc y el cobre: Micronutrientes esenciales para la salud humana. Acta Médica del Centro. 2017;11(2):79-89.
- Borgo F, Riva A, Benetti A, Casiraghi MC, Bertelli S, Garbossa S, et al. Microbiota in anorexia nervosa: The triangle between bacterial species, metabolites and psychological tests. Plos One. 2017;12(6):e0179739.
[Crossref] [Google Scholar] [Indexed]
- Leyrolle Q, Cserjesi R, Mulders MD, Zamariola G, Hiel S, Gianfrancesco MA, et al. Specific gut microbial, biological, and psychiatric profiling related to binge eating disorders: A cross-sectional study in obese patients. Clinical Nutrit. 2021 ;40(4):2035-2044.
[Crossref] [Google Scholar] [Indexed]
- Terry SM, Barnett JA, Gibson DL. A critical analysis of eating disorders and the gut microbiome. J Eat Disord. 2022;10(1):154.
[Crossref] [Google Scholar] [Indexed]
- Prochazkova P, Roubalova R, Dvorak J, Tlaskalova-Hogenova H, Cermakova M, Tomasova P, et al. Microbiota, microbial metabolites, and barrier function in a patient with anorexia nervosa after fecal microbiota transplantation. Microorganisms. 2019;7(9):338.
[Crossref] [Google Scholar] [Indexed]
- Raevuori A, Lukkariniemi L, Suokas JT, Gissler M, Suvisaari JM, Haukka J. Increased use of antimicrobial medication in bulimia nervosa and bingeâ?ÂÂeating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016;49(6):542-552.
[Crossref] [Google Scholar] [Indexed]
- Kleiman SC, Carroll IM, Tarantino LM, Bulik CM. Gut feelings: A role for the intestinal microbiota in anorexia nervosa?. Int J Eat Disord. 2015;48(5):449.
[Crossref] [Google Scholar] [Indexed]
- Dong TS, Mayer EA, Osadchiy V, Chang C, Katzka W, Lagishetty V, et al. A distinct brainâ?ÂÂgutâ?ÂÂmicrobiome profile exists for females with obesity and food addiction. Obesity. 2020;28(8):1477-1486.
[Crossref] [Google Scholar] [Indexed]
- Hankir MK, Patt M, Patt JT, Becker GA, Rullmann M, Kranz M, et al. Suppressed fat appetite after Roux-en-Y gastric bypass surgery associates with reduced brain μ-opioid receptor availability in diet-induced obese male rats. Front Neurosci. 2017;10:620.
- Clark A, Mach N. Exercise-induced stress behavior, gut-microbiota-brain axis and diet: A systematic review for athletes. J Int Soc Sports Nutr. 2016;13:1-21.
[Crossref] [Google Scholar] [Indexed]
- Wells KR, Jeacocke NA, Appaneal R, Smith HD, Vlahovich N, Burke LM, et al. The Australian Institute of Sport (AIS) and National Eating Disorders Collaboration (NEDC) position statement on disordered eating in high performance sport. Br J Sports Med. 2020;54(21):1247-1258.
[Crossref] [Google Scholar] [Indexed]
- Monserrat Hernández M, Arjona Garrido Á, Checa Olmos JC, Salguero García D. Relationship between negative running addiction and eating disorder patterns in runners. Nutrients. 2021;13(12):4344.
[Crossref] [Google Scholar] [Indexed]
- Bamber DJ, Cockerill IM, Rodgers S, Carroll D. Diagnostic criteria for exercise dependence in women. Br J Sports Med. 2003;37(5):393-400.
[Crossref] [Google Scholar] [Indexed]
- Hoek HW. Review of the worldwide epidemiology of eating disorders. Curr Opin Psychiatry. 2016;29(6):336-339.
[Crossref] [Google Scholar] [Indexed]
- Hernández Rodríguez J, Ledón Llanes L, Mendoza Choqueticlla J. Identification and consequences of edorexia. Cuban J Endocrinol. 2018;29(3):1-2.
- Monserrat M, Arjona Garrido A, Checa JC, Salguero D, Tarifa J. Exploratory factor analysis, criterion and psychometric properties of a proposed scale to measure the risk of eating disorders in adolescents (PETCA). Societies. 2023;13(7):156.
- Salguero García D, Montserrat Hernández M. Sports nutrition and dietetics. Dykinson. 2021:120-129.
- Li D, Yu S, Long Y, Shi A, Deng J, Ma Y, et al. Tryptophan metabolism: Mechanism-oriented therapy for neurological and psychiatric disorders. Front Immunol. 2022;13:985378.
[Crossref] [Google Scholar] [Indexed]
- Tardy AL, Pouteau E, Marquez D, Yilmaz C, Scholey A. Vitamins and minerals for energy, fatigue and cognition: A narrative review of the biochemical and clinical evidence. Nutrients. 2020;12(1):228.
[Crossref] [Google Scholar] [Indexed]
- ACSM’s guidelines for exercise testing and prescription, 11th edition. ACSM. 2019.
Author Info
Montserrat Monserrat HERNÁNDEZ1*, Juan Carlos Checa OLMOS2 and Darío Salguero GARCÍA32Department of Social Science, University of Almería, Almería, Spain
3Department of Psychology, University of Almería, Almería, Spain
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
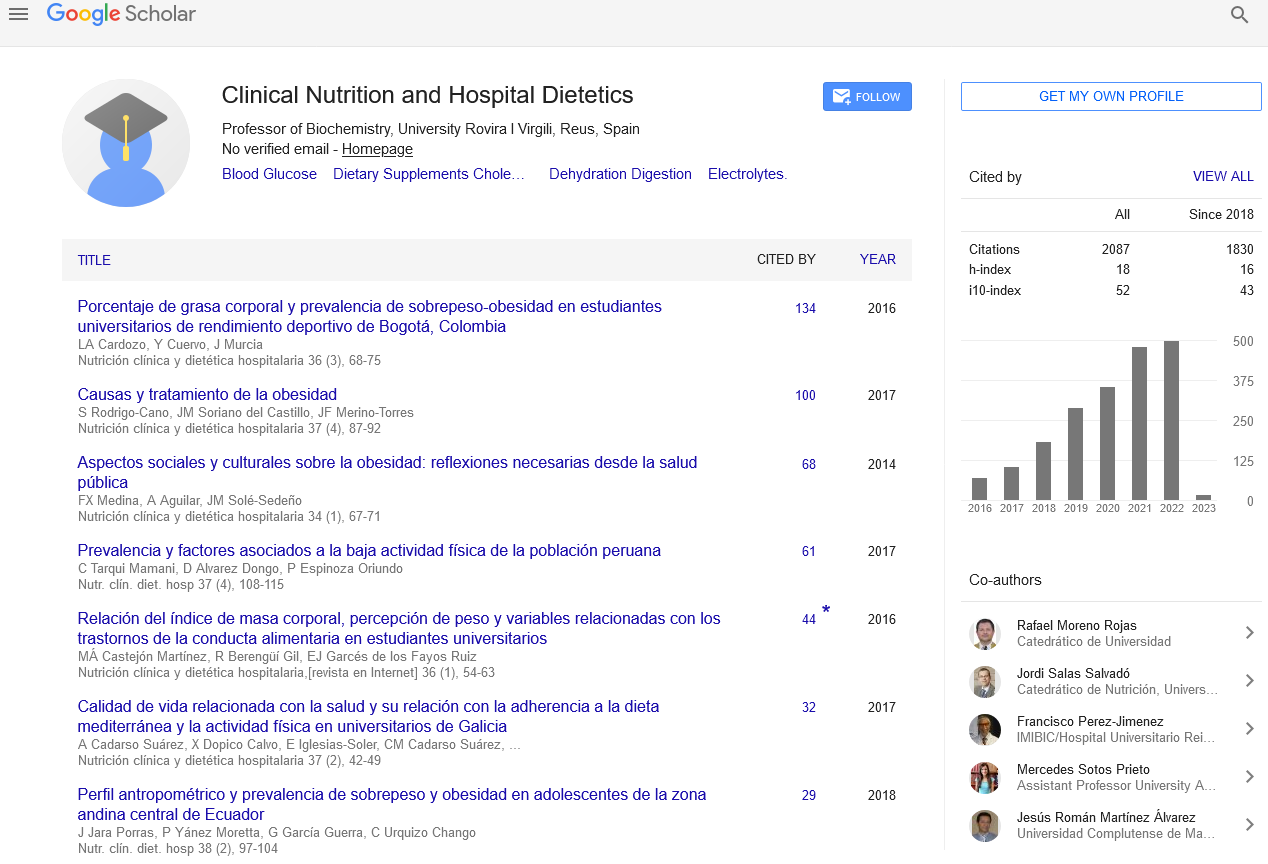
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics